Influence of the First Consultation on Adherence to Antiretroviral Therapy for HIV-infected Patients
Abstract
Background:
Physician attitude influences the way patients cope with diagnosis and therapy in chronic severe diseases such as cancer. Previous studies showed that such an effect exists in HIV care; it is likely that it begins with the first contact with a physician.
Objective:
We aimed to explore in HIV-infected persons their perception of the first consultation they had with an HIV specialist (PFC-H), and whether this perception correlates with adherence to antiretroviral therapy.
Method:
The study was conducted in Grenoble University Hospital, France, a tertiary care center. Every antiretroviral-experienced patient was asked to freely complete a self-reported, anonymous questionnaire concerning retrospective PFC-H, present adherence (Morisky scale), and present perceptions and beliefs about medicine (BMQ scale).
Results:
One hundred and fifty-one questionnaires were available for evaluation. PFC-H score and adherence were correlated, independently from age, gender, and numbers of pill(s) and of pill intake(s) per day. BMQ score also correlated with adherence; structural equation analysis suggested that the effect of PFC-H on adherence is mediated by positive beliefs.
Conclusion:
These results suggest that for HIV-infected persons, the perceptions remaining from the first consultation with an HIV specialist physician influence important issues such as adherence and perception about medicine. Physicians must be aware of this potentially long-lasting effect.
INTRODUCTION
Almost 20 years after the first highly active anti-retroviral combination, 75 to 89% of subjects with a diagnosed HIV infection are treated with antiretroviral therapy (ARV) in western Europe; an undetectable viral load is obtained in 80 to 90% of patients after 6 months of therapy in this area [1]; and several studies suggest that life expectancy of HIV-positive and HIV-negative populations will not differ if ARV are applied early [2].
Therapeutic adherence is a key parameter for the control of the infection, as it is correlated with viral load decrease [3] and CD4+ T cell lymphopenia correction [4]. Besides, a suboptimal adherence enables the emergence of resistant strains of HIV [5], especially in protease inhibitor-free regimens. Due to the integration of HIV genome in the host, such resistant strains persist indefinitely, meaning that the selection of a strain resistant to one or several antiretroviral will definitely prevent the future use of this/these molecule(s) in the future.
Adherence is an important issue in most chronic diseases (for example, diabetes mellitus, seizures or chronic obstructive pulmonary disease); however, there are many different barriers or challenges that HIV-positive patients may specifically experience when they try to adhere to their medication regimen. First, historical stigmas associated with AIDS probably restrain adherence and access to health care. Second, several national guidelines (including 2013 French guidelines [6]) recommend initiating antiretroviral medication as soon as possible after the diagnosis of HIV infection, regardless of the viral load, CD4 T cell count or clinical stage of the disease. This implies to treat asymptomatic individuals, who could underestimate the importance of adherence.
The impact of different factors on therapeutic adherence has been explored in many studies. For example, poor adherence has been shown to be associated with young age [7], psychiatric and neurological disorders [8, 9]), and addiction [10]. Conversely, other factors such as family support [11] have a positive impact on adherence. Gender [12] and ethnicity have an inconstant effect, depending on the studies. For example, a study in Greek subjects older than 50 years did not identify a strong link between gender and adherence to ARV therapy [13], and a study in US adult subjects did not identify gender-related differences in adherence. On the contrary, a study in US HIV-infected IV drug users observed a lower adherence in women [14]; and another study in a similar population observed that alcohol consumption was associated with a lower adherence in women but not in men [15]. The treatment regimen (daily number of pills and daily intake) [7] and side effects of the antiretroviral therapy [16] may also influence adherence. Finally, studies showed that therapeutic adherence is influenced by patient-physician relationship, including provision of HIV-specific information, egalitarian decision-making style, and trust in the physician. For example, a study in Mexico observed that adherence in the past month was lower in patients who were not satisfied of the relationship with their physician [17]; in a US study, adherence was lower in case of mismatch between the patient's expectations of care and the physician's consultation style [18]; another study observed that several dimensions of the physician-patient relationship (general communication, HIV-specific information, participatory decision making, overall physician satisfaction, willingness to recommend, physician trust, and adherence dialogue) were associated with adherence [19]. Interestingly, in another study [20], US patients declared that the progresses they made concerning their adherence were not due to their healthcare providers, but that they appreciated providers who knew and cared about their personal lives, who were clear and direct about instructions, and who were accessible. These last results suggest that this type of physician-patient relationship may sometimes acts indirectly.
To establish this kind of patient-physician relationship should be a goal from the first consultation, that is, during the announcement of a positive HIV test, or when the initiation of ARV is discussed. In other disciplines, particularly oncology, efforts have been made to codify important steps such as diagnosis and treatment discussions. Indeed, it has been shown that the way a cancer diagnosis is disclosed deeply influences the patient perception of the disease and of the therapy [21-24]; furthermore, announcing a cancer diagnosis is known to require specific skills and formation [25, 26]. It is likely that this announcement is similarly decisive in HIV-infected patients, but studies assessing the influence of the first consultation with an HIV-specialist physician on outcome are lacking. One should nevertheless note that the Voluntary Counseling and Testing and HIV testing and Consulting approaches have not only demonstrated to positively influence at-risk behavior [27], but also to adherence [28]. More specifically, to our knowledge, no study has analyzed the relationship between the experience of the patient during the first consultation with an HIV specialist physician, and adherence to ARV.
Our objective was therefore to explore the relationship between the patient perception of this first consultation and subsequent adherence. More precisely, we aimed to determine whether positive perceptions of this first consultation were correlated with a present better adherence, and whether more general perceptions concerning treatments and medicine help understanding this correlation.
MATERIALS AND METHODS
Study Population
The study was conducted from May to July 2014, in the University Hospital of Grenoble, France, a tertiary care hospital. About 900 HIV-infected adults regularly attend this center, with 4 to 10 visits per year for follow-up and ARV prescription. Every HIV-infected patient under ARV who visited the infectious disease unit (mostly for blood tests and consultation) during the study period was asked to freely fill a self-administered questionnaire. No mention of the patient identity was required, and anonymity was maintained by participants placing the completed questionnaire in an urn in the waiting room.
The study was conducted according to the principles of the declaration of Helsinki. Ethical approval was obtained from the Comité d’Ethique pour les Recherches Non Interventionnelles of Université Grenoble Alpes (advice N° 2014-05-13-45).
Questionnaires
Beliefs about Medicine Questionnaire (BMQ)
The BMQ is an 18-item scale examining the perception of the patient regarding treatments and medicine [29]. This scale has been validated in HIV infection context [30] and validated in French language [30]. The first two parts explore the positive (“necessity”) and negative (“concerns”) perception of ARV therapy, and the last two parts explore the general negative beliefs concerning drug prescription by physicians (“overuse”) and concerning medications (“harm”). The value of each of the four dimensions of the beliefs about medicine is obtained by summing the numbers attributed to each question (from 1 for “totally disagree” to 5 for “totally agree”).
Adherence
We used the Morisky-8-item Adherence scale. It has been widely used for the assessment of adherence in different diseases, and has already been validated in the case of antiretroviral therapy [31].
Although they may overestimate the percentage of properly taken medications, self-administered questionnaires have been shown to be a valid way to approximate adherence, and to be correlated with viral load [32] or measurements established with microelectronic monitoring system.
Patient Perception of the First Consultation with an HIV Specialist Physician (PFC-H)
The perception of the first consultation with an HIV specialist physician (PFC-H) was evaluated with a set of 16 questions (see supplementary material). Closely related questions have been validated in HIV-infected patients [30] and have been adapted to fit to the topic of the present study (the first consultation). These questions explore the perception concerning the meeting and the attitude of the physician. Patients were asked to evaluate (no, mostly no, mostly yes, yes) items such as “Did you feel like the physician told you all the truth?”, “Did the physician encourage you to express yourself?”, “Did the physician carefully listen to you?”, “Was the physician respectful?”, or ”Did you feel like the physician understood you?”. The answers were graduated on a 1-to-4 scale (No, Rather no, Rather yes, Yes), and the PFC-H score was calculated by summing the answer to each of the 16 questions.
Statistical Analysis
Missing values were imputed using an iterative Markov Chain Monte Carlo (MCMC) method [33]. Categorical data are reported as frequency and percentage and continuous data as mean and standard deviation. Pearson’s coefficient was used for correlations between scores.
The influence of the various dimensions of BMQ and of PFC-H on adherence was tested with multiple linear regression analysis. In order to assess the potential mediation of positive beliefs to explain the effect of PFC-H on adherence, post hoc structural equation modeling was performed.
Direct and indirect effects and bias-corrected p-value for the indirect effect were computed by bootstrapping. We considered p-values <0.05 as significant. Statistical analysis was performed with SPSS® and SPSS® Amos 22 for Windows (IBM, Inc., Armonk, New York, USA).
RESULTS
Among the 270 patients who visited our center during the 4-months study period, 161 participated. One hundred and fifty-one questionnaires were eventually analyzable; ten questionnaires were too incompletely filled in key sections to be included in the study. Across the 151 analyzable questionnaires, 4.1% of the survey items were missing and treated as described. Patients were aged 48±11 years and were predominantly male (78.1%); 63.8% identified themselves as men having sex with men (MSM). Most (86%) of the patients were Caucasians. Many patients (84.8%) reported having an undetectable HIV plasma viral load (<20 copies/ml), and 53.3% reported having a CD4 T cell count above 500/mm3. The first consultation with an HIV specialist physician had occurred 14.1±8.4 years (mean±SD) before the present study (5 years or less for 20.8%, 20 years or more for 34.3%).
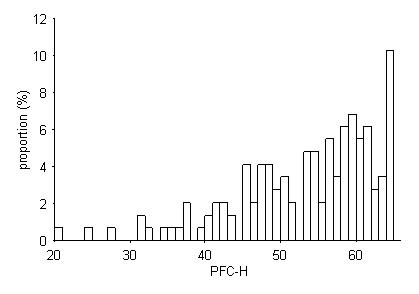
Mean PFC-H score was 54.2 ± 8.3 (20-64). It was 60 or more for 46 (30.4%) patients, and less than 40 for 13 (8.6%) patients (Fig. 1). It was not correlated with age, and was not different in female vs. male or in men having sex with men vs. other patients. It was negatively correlated with the time elapsed since the first consultation (r=-0.28, p<0.01).
| Scale | Score [mean±SD] (minimal and maximal possible) | Correlation with Morisky adherence scale | ||
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| R | p-value | p-value | ||
| PFC-H | 54.2 ± 8.3 (16-64) | 0.214 | 0.01 | 0.25 |
| BMQ Necessity | 22.7 ± 3.1 (5-25) | 0.308 | <0.001 | 0.04 |
| BMQ Concerns | 13.2 ± 4.3 (5-25) | -0.270 | 0.001 | 0.09 |
| BMQ Overuse | 7.2 ± 2.9 (4-20) | -0.238 | 0.003 | 0.94 |
| BMQ Harm | 10.4 ± 4.2 (4-20) | -0.267 | 0.001 | 0.23 |
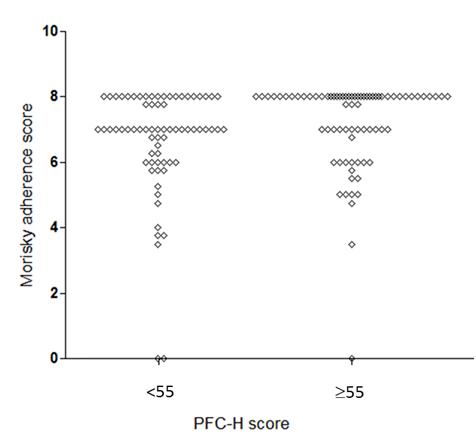
Adherence was high, with 43.7% patients, 28.9% and 14.0% having a Morisky adherence score of respectively 8/8, 7/8 and 6/8. We observed an association between PFC-H and Morisky adherence score. First, when taking as a cut-off the median value of PFC-H score (55), we observed that 71.4% and 44% of the patients with a PFC-H <55 and ≥55, respectively had a Morisky adherence score below 8 (p<0.01) (Fig. 2). Second, Morisky adherence score was correlated with PFC-H score in univariate analysis (R=0.21; p=0.01) (Table 1), and remained correlated when adjusting for age, gender, current numbers of pill(s) per day, current number of pill intake(s) per day, and comorbidities (p=0.02). The Morisky adherence score and the time elapsed since the first consultation were not correlated (p=0.51). Adherence was also correlated with the four dimensions of the BMQ (Table 1).
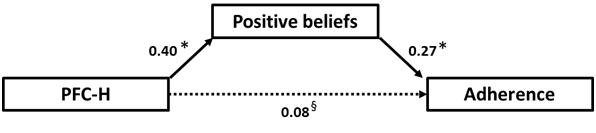
In a multiple linear regression model integrating PFC-H and BMQ scales, one of the dimensions of the BMQ score (positive beliefs, or “BMQ necessity”) was still significantly associated with Morisky adherence score, but not PFC-H. To determine whether PFC-H may have an influence on adherence via positive belief, we elaborated a post hoc structural equation model. The results showed that the effects of PFC-H on adherence are likely to be fully mediated by positive beliefs (Fig. 3) (p<0.01 and p=0.32 for indirect and direct effects of PFC-H on adherence, respectively).
DISCUSSION
In developed countries, thanks to antiretroviral therapy, HIV infection has become for most patients a chronic state rather than a chronic disease. When antiretroviral therapy is prescribed, a health condition compatible with, for example, professional activity is generally regained or maintained. Adherence to treatment is a key parameter to reach and to maintain this situation. We wanted to determine whether adherence was associated with the perceptions of the first consultation with an HIV specialist (PFC-H).
The score we elaborated to retrospectively evaluate the PFC-H revealed generally positive perceptions, although the value was clearly low in some cases. This is not a totally new score, as these questions have already been tested in HIV-positive patients in a previous work [30], although without assessing specifically the perception of the first consultation. This score may therefore require to be validated in other HIV-positive populations.
We observed a significant association between present adherence and the perceptions of this first meeting. Although adherence was generally high in our population, patients with positive perceptions had an even higher adherence. To our knowledge, the present study is the first to explore this dimension in HIV-infected patients. These results are consistent with previous studies that showed that the quality of the information delivered by the caregiver, and the way the caregiver behaves with the patient, influence the adherence to HIV care [34], or to diabetes care in patients with type 2 diabetes [35], or to therapy in patients with multiple sclerosis [36]. The influence of the physician-patient relationship has also been extensively studied in cancer patients. Indeed, it has been shown [22] that the experience of these patients during the disclosure was intense, and that it influenced the future perception of the disease and of the treatment. It is therefore not unlikely that for HIV patients, the first consultation with an infectious disease specialist will similarly impact adherence. Physicians should be aware of the future influence of this consultation, and behave consistently, i.e. providing patients the optimal information, support and listening time. The success of communication skills training programs for oncologists [25] may pave the way to similar training programs intended to HIV caregivers.
In a regression model including BMQ and PFC-H, the last did not appear to be associated with adherence independently of the first. However, between two perceptions so close in their topics, it may be less justified to speak in terms of dependency or independency. We therefore used a structural equation model; the model which fit the best with the data we had collected was an indirect effect of PFC-H on adherence via an effect on positive beliefs concerning medicine. This result describes in a more satisfying way the interplay between PFC-H, perceptions concerning medicine, and adherence than the regression model. It suggests that PFC-H has an important influence on the considerations the patient will develop regarding medicine and treatment, and therefore on adherence. Again, this indicates that physicians should behave carefully during their first consultation with an HIV-infected subject, as the patient perceptions may have a persisting influence.
Our study has several limitations, the most important being the important mean time elapsed since the first consultation; after such a delay, the memories of the analyzed perceptions may have been modified. The negative correlation we observed between PFC-H and the time elapsed since the first consultation is maybe an illustration of this memory bias concerning the first consultation, which occurred in some patients more than 20 years ago, although it may also reflect the fact that recent first consultations fill more the patient expectations than before. Another limitation is the purely declarative information on adherence, reason why we chose not to assess the impact of the dimensions we explored on self-reported clinical and biological outcomes. Finally, the analyzed population through questionnaire filling was not representative of the whole cohort consulting at our institution, being more Caucasian and masculine. This sample population may have different expectations and perception from physician-patient interactions.
CONCLUSION
Our study suggests that the first meeting between an HIV-infected adult and an HIV specialist physician positively influences adherence, especially through perceptions on medicine and ARV. Physicians should be aware of what is at stake during this first consultation, and be trained accordingly to provide relevant information, listening time, respectful attitude, and to involve the patient in the decision process.
LIST OF ABBERIVATIONS
| ARV | = Antiretroviral therapy |
| BMQ | = Beliefs about Medicine Questionnaire |
| PFC-H | = Perceptions of the first consultation with an HIV specialist |
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publishers Website along with the published article.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank all the physicians that participated in the study.


