All published articles of this journal are available on ScienceDirect.
Correlates of HIV Infection Among Sexually Active Adults in Kenya: A National Population-Based Survey
Abstract
Objective:
To identify factors associated with prevalent HIV in a national HIV survey in Kenya.
Methods:
The Kenya AIDS Indicator Survey was a nationally representative population-based sero-survey that examined demographic and behavioral factors and serologic testing for HIV, HSV-2 and syphilis in adults aged 15-64 years. We analyzed questionnaire and blood testing data to identify significant correlates of HIV infection among sexually active adults.
Results:
Of 10,957 eligible women and 8,883 men, we interviewed 10,239 (93%) women and 7,731 (87%) men. We collected blood specimens from 9,049 women and 6,804 men of which 6,447 women and 5,112 men were sexually active during the 12 months prior to the survey. HIV prevalence among sexually active adults was 7.4%. Factors independently associated with HIV among women were region (Nyanza vs Nairobi: adjusted OR [AOR] 1.6, 95%CI 1.1-2.3), number of lifetime sex partners (6-9 vs 0-1 partners: AOR 3.0, 95%CI 1.6-5.9), HSV-2 (AOR 6.5, 95%CI 4.9-8.8), marital status (widowed vs never married: AOR 2.7, 95%CI 1.5-4.8) and consistent condom use with last sex partner (AOR 2.3, 95%CI 1.6-3.4). Among men, correlates of HIV infection were 30-to-39-year-old age group (AOR 5.2, 95%CI 2.6-10.5), number of lifetime sex partners (10+ vs 0-1 partners, AOR 3.5, 95%CI 1.4-9.0), HSV-2 (AOR 4.7, 95%CI 3.2-6.8), syphilis (AOR 2.4, 95%CI 1.4-4.0), consistent condom use with last sex partner (AOR 2.1, 95% CI 1.5-3.1) and lack of circumcision (AOR 4.0, 95%CI 2.8 - 5.5).
Conclusion:
Kenya’s heterogeneous epidemic will require regional and gender-specific prevention approaches.
INTRODUCTION
Lack of a comprehensive understanding of national HIV epidemics remains a major challenge for targeting effective HIV programs. Antenatal clinic (ANC) sentinel surveillance has been useful to document trends of generalized epidemics but lacks adequate sexual-behavioral and other associated risk factors for HIV infection, and is not generalizable to men and non-pregnant women [1]. Studies conducted in a number of sub-Saharan African countries showed that ANC data over-estimated prevalence in 15-19 year olds and underestimated prevalence in older ANC clinic attendees [2, 3]. Hospital-based studies have also been conducted in low prevalence areas to understand risk factors [4], but the findings are not easily generalizable to populations living in countries with high HIV prevalence.
Concerns about the representativeness and accuracy of national HIV estimates derived from ANC surveillance have led to an increased demand for surveys and more data on the prevalence and distribution of HIV in the whole population [5]. In sub-Saharan Africa, more than 38 countries have conducted national population-based HIV surveys [6]. These surveys most often were restricted to reproductive ages, collected dried blood spots for biological tests [7], and avoided questions about sexual behavior and HIV status which are considered sensitive. Thus, laboratory and risk factor analyses have been limited. Programmatic data from voluntary counseling and testing (VCT) centers as well as HIV test results from prevention of mother-to-child transmission (PMTCT) programs have been used in some cases to estimate HIV prevalence and investigate associations with demographic, behavioral, and biological factors [8-10]. However, these are limited due to their lack of representativeness of the populations that seek VCT and PMTCT services [11]. For example, PMTCT services are only offered to pregnant women. Additionally, risk behavior, perception of risk behavior, or attitudes towards HIV/AIDS have been shown to influence uptake of VCT services [12].
Sexual transmission is the major route for HIV infection in sub-Saharan Africa [13,14]. In Kenya, sexual transmission contributes over 90% of all HIV infections [13]. The World Health Organization (WHO) categorizes Kenya as having a generalized HIV epidemic, defined as having an HIV prevalence of more than 1% in the adult general population and more than 5% in vulnerable adults such as sexually transmitted infection (STI) clinic patients. Kenya has wide variability in the distribution of HIV infection by geographic, demographic, sexual-behavioral, and biological factors. The Kenya Demographic and Health Survey (KDHS) conducted in 2003 included HIV serology but was limited in the scope and depth of sexual-behavioral and biological indicators collected, and included consenting adults aged 15-49 years [15]. In this era of expansion of prevention, care and treatment programs for HIV, additional variables of interest are needed to facilitate accurate interpretation of HIV prevalence data and associated risk factors [16].
We conducted the Kenya AIDS Indicator Survey (KAIS) in 2007 to provide nationally-representative and comprehensive data on demographic, behavioral, and biologic indicators of HIV/AIDS, beyond that of previous national HIV surveys in Kenya. In addition to providing national prevalence estimates for HIV and sexually transmitted infections, these data provided the opportunity to link HIV status with key demographic, behavioral, and biologic information to identify significant correlates associated with HIV infection in Kenya. We examined factors independently associated with the risk of HIV infection among individuals who were sexually active during the 12 months prior to the survey.
METHODS
Ethics Statement
Ethical approval was obtained from the Ethical Review Committee at the Kenya Medical Research Institute (KEMRI) and the Institutional Review Board at the Centers for Disease Control and Prevention (CDC). Respondents provided consent separately for the interviews and blood draws.
Study Setting
KAIS was conducted among a nationally representative sample of households selected from all the eight provinces in Kenya, covering both rural and urban areas. Various studies show that Nyanza province continues to have the highest HIV prevalence in Kenya [15,17,18]. Nairobi province is the capital city and has a cosmopolitan population with diverse ethnic groups and cultures. Nyanza on the other hand is predominantly inhabited by the Luo ethnic group.
Survey Design, Sampling and Participation
Briefly, we conducted a cross-sectional, stratified two-stage cluster survey designed to achieve a nationally representative sample and sufficient statistical power to provide prevalence estimates for each of the 8 provinces (Fig. 2). The first stage involved selecting 415 clusters out of 1,800 in the national sampling frame and the second stage involved the selection of households per cluster with equal probability of selection in the rural-urban strata. In order to reflect the population distribution, we sampled 294 and 121 clusters in rural and urban areas respectively. We collected data between August and December, 2007. Eligible participants were individuals aged 15-64 who were residents or household visitors the night prior to the survey team’s visit. We administered household and individual questionnaires and collected venous blood from respondents. Key questions included respondent’s HIV status, testing history, age at sexual debut, condom use, number of lifetime sex partners, alcohol use during last sexual intercourse, male circumcision status and mobility (which was defined as the number of separate occasions when the respondent traveled away from home/community and slept away in the previous 12 months) and access to cotrimoxazole and antiretroviral therapy (ART) for those with HIV infection. Partner-specific information on HIV status, testing history, disclosure, condom use and family planning preference were collected for up to four sex partners in the last year. With exception of condom use and family planning preferences, many of the indicators were unique to KAIS and were not asked in the KDHS. For population size estimates, we used census data from the Kenya National Bureau of Statistics, using the 2006 sampling frame based on the 1999 census. We calculated the corresponding 95% confidence intervals taking into account the sampling weights and study design. Full details of methods used in KAIS have been published elsewhere [18].
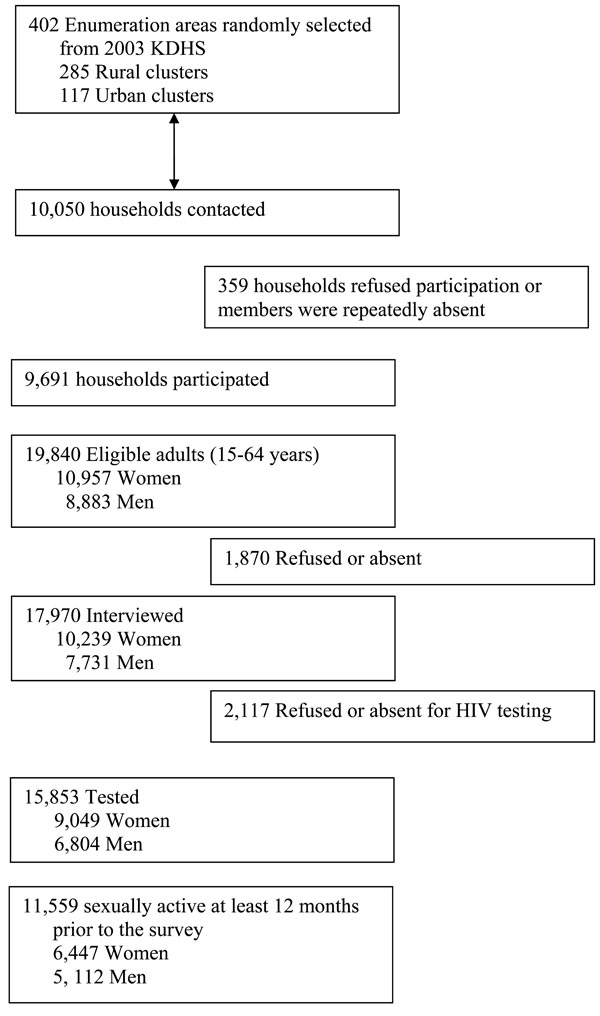
Study Profile.
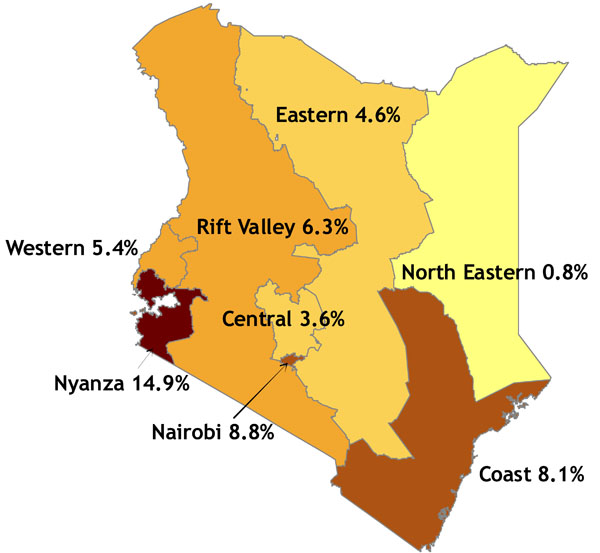
Map of Kenya, with provincial HIV prevalence among all adults aged 15-64 years.
Laboratory Testing
Blood specimens were transported to Kenya’s National Public Health Laboratory in Nairobi and tested for HIV, syphilis and HSV-2. CD4 cell count enumeration was conducted for HIV-infected participants. HIV testing was performed according to the national guidelines for HIV testing using a validated HIV testing algorithm for the country: the Vironostika HIV Uni-Form II antigen/antibody (BioMérieux Bv, Boseind, Netherlands) for screening and the Murex HIV antigen/antibody combination (Abbott/ Murex-Biotech Ltd, Kent, UK) for confirmation in a serial testing algorithm. Specimens with discordant results were re-tested with the two assays. Polymerase Chain Reaction (PCR) testing was conducted on specimens that still had two discordant results after re-testing. For HSV-2 testing, the Kalon HSV Type 2- specific IgG EIA (Kalon Biologicals, Guildford, UK) was used; this was a recombinant type 2 antigen (gG2) modified to eliminate reactivity arising from HSV type 1 infection, at the same time retaining the natural antigenic characteristics of HSV-2. For syphilis infection, serum specimens were first screened using a Treponema pallidum particle agglutination assay (TPPA) (Serodia-TPPA, Fujirebio Diagnostics Inc, Tokyo, Japan) to detect previous exposure to syphilis antigens. All TPPA-positive specimens were then tested using a rapid plasma reagin (RPR) (Becton, Dickinson and Company, Franklin Lakes, NJ, USA) test on undiluted (i.e. neat) serum specimen to test for reaginic antigens. Specimens with positive TPPA and RPR serologies were defined an active syphilis infection. For quality control of each test, all positive specimens and 5% of negative specimens were retested in a different laboratory using the same testing algorithms.
Data Analysis
Data from questionnaires were entered into a CSPro database (version 3.3, US Census Bureau, Washington DC, USA) by two different data clerks. All discrepancies between the two entries were resolved by a data manager during the data cleaning stage. To obtain nationally representative estimates, we calculated sampling weights for each individual and household based on selection probability and taking into account cluster-level non-participation. In addition, special weights were calculated for those who participated in the blood draw to take into account cluster-level non-participation.
For the purposes of this paper, we restricted analysis to a sub-set of questions from the individual questionnaire among participants who were sexually active in the last year before the survey. Sexually active individuals were those who self-reported having had sexual intercourse. Additionally, we conducted a sub-analysis to further investigate correlates of HIV infection that were specific to Nyanza province, the province with the highest HIV prevalence rate for men and women compared to all other provinces. We used the Rao-Scott chi-square test which allowed adjusting for the cluster survey design when testing for associations between categorical variables and HIV infection. Bivariate analysis was used to quantify the association between the demographic, behavioral and biological variables and HIV infection. We conducted multivariate logistic regression by constructing separate models for males and females to assess factors independently and significantly associated with HIV infection among sexually active persons. All variables were first included in the models and model selection was carried out using a backward elimination procedure. All variables that had a p-value of greater than 0.5 were removed from the models in the first step unless they were suspected to be confounders. Variables were then removed sequentially from the models starting with the one with the highest p-value until all variables had a p-value of less than 0.05. All confounders were retained in the model irrespective of the p-value. Odds ratios, adjusted odds ratios (AOR), and associated 95% confidence intervals were calculated based on pre-specified reference groups.
RESULTS
We collected information from 9,691 households. A total of 19,840 individuals were eligible, of which 17,970 (90%) consented to be interviewed, including 10,239 women (93%) and 7,731 men (87%) (Fig. 1). Among the eligible respondents, 9,049 (83%) women and 6,804 (77%) men consented for and provided a blood sample for HIV, HSV-2, and syphilis testing, a response rate of 88% of those interviewed, with similar uptakes rates among men and women. Among those consenting to blood draw 6,447 women (71%) and 5,112 men (75%) were sexually active in the last year. Overall, 57% of KAIS participants were female, the median age was 30 years, 74% resided in rural areas, 70% were currently employed, 61% were married, and <1% of women and 6.6% of men drank alcohol before their last sexual encounter (Table 1). Among the laboratory-confirmed HIV positive respondents, 56% had never tested for HIV infection, 28% self-reported HIV negative and 16% self-reported HIV positive status. We found ethnicity to be co-linear with province and circumcision and choose to present differential risks with a focus on circumcision status and province rather than with a focus on ethnicity.
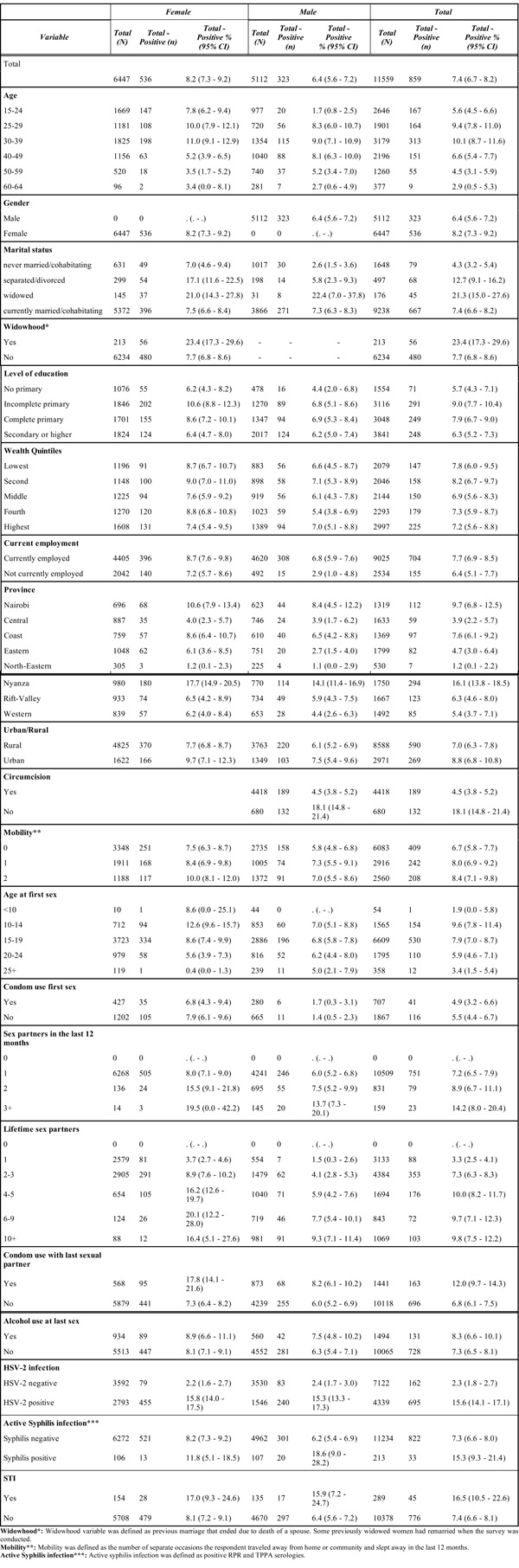
HIV Prevalence by Demographic, Behavioral and Biologic Factors Among Sexually Active Adults Aged 15-64 Years in Kenya in 2007
 |
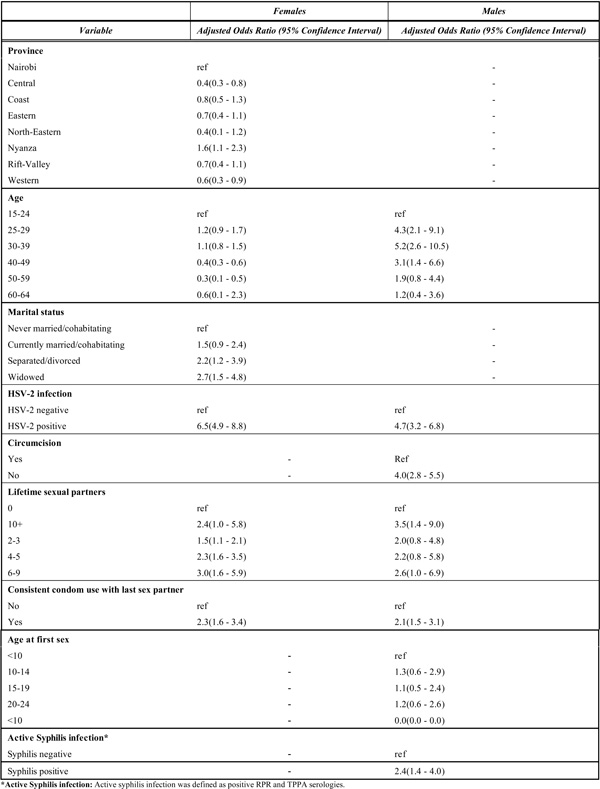
Factors Independently Associated with HIV Infection Among Sexually Active Adults in Kenya in 2007
 |
HIV Prevalence
Overall, HIV prevalence among all adults aged 15-64 years was 7.1% (95% CI, 6.5-7.7), representing an estimated 1.4 million people nationwide. Among sexually active adults aged 15-64 years old, 7.4% (95% CI, 6.7-8.2) were infected with HIV. Women were more likely to be infected (8.2%) than men (6.4%). Young women aged 15-24 years were nearly 5 times more likely to be infected (7.8%) than young men of the same age group (1.7%). HIV prevalence increased with age, with the highest prevalence (10.1%) between 30 and 39 years. Among 30-39 year olds, HIV prevalence was 11.0% among women compared to 9.0% among men. Prevalence among individuals aged 60-64 was 2.9%.
Although there was no difference in HIV prevalence between rural and urban areas,, prevalence varied greatly across provinces (Table 1). Women had higher HIV prevalence than men in all provinces. In Nyanza Province 17.7% (95% CI, 14.9-20.5) of women and 14.1% (95% CI, 11.4-16.9) of men were infected. HIV prevalence was higher among married or cohabitating (7.4%, 95% CI 6.6-8.2), separated/ divorced (12.7%, 95% CI 9.1-16.2), and widowed individuals (21.3%, 95% CI 15.0-27.6) compared with never married individuals (4.3%, 95% CI 3.2-5.4). We observed no difference in HIV prevalence by wealth status for women and men; however, men who were currently employed had higher prevalence (6.8%, 95% CI 5.9-7.6) than those that were not employed (2.9%, 95% CI 1.0-4.8) (Table 1).
Behavioral Factors and HIV Infection
Among sexually active men, HIV prevalence was 18.1% (95% CI 14.8-21.4) among uncircumcised men and 4.5% (95% CI 3.8-5.2) among the circumcised men. HIV prevalence in uncircumcised men rose sharply between the 15-24 year age group (3.2%) and the 30-39 year age group (30.4%) and remained high in uncircumcised men through age 59.
Among participants who reported being sexually active in the last 12 months, consistent condom use with the last sex partner was associated with higher HIV prevalence compared to no condom use with the last sex partner (Table 1). However, a sub-analysis showed that HIV-infected persons who knew their sero-positive status were 4 times more likely to use a condom compared to those who self-reported an HIV negative status based on the result of their last test (53.1.% vs 13.9%) or those who had never had an HIV test (11.2%).
HIV prevalence also varied with STI infection. Respondents who reported any STI in the last 12 months had higher prevalence of HIV (16.5%) compared to those not reporting an STI (7.4%), and 44.7% of women and 32.0% of men were infected with HSV-2. HIV prevalence among those co-infected with HSV-2 was 15.6% compared to 2.3% among those not infected with HSV-2. Syphilis prevalence was 1.9% (1.6% and 2.3% among women and men, respectively). HIV prevalence was significantly higher among those infected with syphilis (16.5%) compared to those without syphilis infection (7.4%).
Factors Independently Associated with HIV
Women
In multivariate analyses, independent correlates of HIV infection among sexually active women were geographical area of residence (Nyanza Province vs Nairobi: adjusted OR [AOR] 1.6, 95% CI 1.1-2.3), higher number of lifetime sex partners (6-9 vs 0-1 partners: AOR 3.0, 95% CI 1.6-5.9), HSV-2 infection (AOR 6.5, 95% CI 4.9-8.8), marital status (separated/divorced vs never married: AOR 2.2, 95% CI 1.2-3.9; widowed vs never married: AOR 2.7, 95% CI 1.5-4.8) and consistent condom use with the last sex partner (AOR 2.3, 95% CI 1.6-3.4) (Table 2).
Men
Among men, correlates of HIV infection were age group (30-39 years vs 15-24 years: AOR 5.2, 95% CI 2.6-10.5), number of lifetime sex partners (≥10 partners vs 0-1, AOR 3.5, 95% CI 1.4-9.0), HSV-2 infection (AOR 4.7 95% CI 3.2-6.8), syphilis infection (AOR 2.4, 95% CI 1.4-4.0), consistent condom use with the last sex partner (AOR 2.1, 95% CI 1.5-3.1) and lack of male circumcision (AOR 4.0, 95% CI 2.8 - 5.5) (Table 2).
Factors Associated with HIV in Nyanza Province
Prevalence among sexually active adults in Nyanza province was highest in the 25-to-29-year-old age group for women (23.4%) and in the 30-to-39-year old age group for men (25.9%). Of separated/divorced individuals, 42.2% were HIV-infected; uncircumcised men had a prevalence of 20.8% compared to the 6.8% among those circumcised. In multivariate analysis, factors independently associated with HIV prevalence among recently sexually active women were age group 25-29 years vs 15-24 years (AOR 1.3, 95% CI 0.8-2.3); current marital status (separated/divorced vs never married: AOR 5.7, 95% CI 1.5-20.9; widowed vs never married: AOR 4.4, 95% CI 1.0-19.5), HSV-2 infection (AOR 6.4, 95% CI 3.6-11.4), higher number of lifetime sex partners (6-9 vs 0-1: AOR 3.2, 95% CI 1.2-9.0), consistent condom use with the last sex partner (AOR 3.2, 95% CI 1.9-5.5), mobility (2 days vs 0 days: AOR 1.4, 95% CI 0.9-2.3). Factors associated with HIV infection among recently sexually active men were age group 30-39 years vs 15-24 years (AOR 19.1, 95% CI 5.9-61.6); education (incomplete primary vs no primary: AOR 1.4, 95% CI 0.5-4.0), HSV-2 infection (AOR 4.6, 95% CI 2.2-9.4), consistent condom use with the last sex partner (AOR 3.7, 95% CI 2.0-7.1), and lack of male circumcision among men (AOR 2.8, 95% CI 1.7-4.8).
DISCUSSION
In 2007, an estimated 7.4% of sexually active Kenyan adults aged 15-64 years were infected with HIV. Correlates of HIV infection among women and men were age, number of lifetime sex partners, residence in Nyanza province, HSV-2 infection, consistent condom use with the last sex partner and lack of circumcision among men. The strongest independent predictors for HIV infection for both women and men were HSV-2 co-infection and higher number of lifetime sex partners.
HIV prevalence was highest in Nyanza Province, where 16.9% of the sexually active adults were HIV-infected. In a sub-analysis for Nyanza Province, we found that age, HSV-2 infection, multiple lifetime sex partners, consistent condom use with the last sex partner and lack of male circumcision were independently associated with HIV. Many of these factors are similar to predictors of HIV infection found at the national level and are consistent with findings from other studies [1,8,16,19].
In Kenya, the adjusted odds of having HIV among sexually active persons with HSV-2 infection were 5-6-fold higher than those uninfected with HSV-2. However, awareness of HSV-2 is very low, even among health care providers, despite the high prevalence of HSV-2 and the potential role of HSV-2 in driving the HIV epidemic [20,21]. HIV-induced immune compromise can result in frequent and persistent HSV disease, while poorly managed HSV replication may influence HIV transmission [22]. Researchers estimate that in settings with high HSV-2 prevalence, such as Nyanza province, HSV-2 infection could contribute to the risk of HIV-infection in more than one in four new cases of HIV [19,21]. Unfortunately, randomized controlled trials that have examined daily acyclovir treatment of HSV-2 among persons with HIV co-infection, or acyclovir prophylaxis among persons without HIV have not demonstrated a protective effect [23].
The results from KAIS show a non-statistically significant increase in overall HIV prevalence from KDHS 2003 (7.4% vs 6.7%) among those aged 15-49. The potential increase in HIV prevalence may be in part due to the survival effects of antiretroviral therapy. It may also indicate increasing incidence and a need to improve and expand HIV prevention programs throughout Kenya, and particularly in Nyanza Province. Appropriate messages on delaying sexual debut, knowledge of HIV status, male circumcision, consistent and correct use of condom with partner of unknown HIV status or known discordant HIV status, and reduction of number of sex partners should be reinforced [8, 24, 25]. Our study showed that widowhood and divorce were significantly associated with higher HIV prevalence. This corroborates findings from other sub-Saharan African countries which show that women who encounter marital disruption through divorce or widowhood were more likely to be HIV infected [26]. On the other hand, divorce is more common among HIV-infected women, particularly those in HIV discordant unions [27].
Ethnicity and province influence both the distribution of circumcision practice and HIV prevalence. Several studies have showed that male circumcision reduces the risk of HIV acquisition among men [28]. High prevalence in Nyanza province could be attributed to low male circumcision rates. Among the general population, 85% of men were circumcised nationally while 48.2% were circumcised in Nyanza Province. In addition, cultural practices such as widow inheritance practiced among the Luo community (the predominant ethnic group in Nyanza) may be a factor [28, 29]. Widow inheritance is a traditional practice in which a designated man takes social and economic responsibility over a woman following the death of her husband [30]. A study by Agot et al. [30] in Nyanza province showed that inherited widows were more likely to have HIV infection compared to those not inherited. Luo women are believed to acquire contagious cultural impurity following the death of a husband. Often, a professional “cleanser” is hired who performs sexual rituals to cleanse the widow. If the spouse of the deceased is HIV-infected, the cleanser acts as a bridge for HIV transmission to other widows hence putting widowed women at a high risk [31]. The Kenya Ministries of Health published The National Guidance for Voluntary Medical Male Circumcision (VMMC) in January 2008 and in November 2008 launched the VMMC program focusing on Nyanza province and other traditionally non-circumcising communities with the aim of reducing new HIV infections and other STIs. The guidance provides a broad policy framework for the integration of VMMC into existing HIV prevention programs.
Respondents reporting ever having used condoms were more likely to have HIV infection. Condom use reduces risk of HIV acquisition and transmission [32] and HIV-infected persons who are aware of their HIV infection are more likely to use condoms [33, 34]. KAIS showed a 4-fold increase in condom use among those who knew their HIV-positive status. Though the association between condom use and HIV infection was not expected, the finding may reflect the success of positive prevention interventions and condom promotion efforts to increase condom use by people living with HIV. These data highlight the need for future HIV surveys to collect more detailed partner-specific information on condom use and knowledge of HIV status of participants and their partners which could help interpret the complex associations between condom use, sexual behavior, and HIV. The application of a laboratory assay that can accurately distinguish recent from established infection could also suggest the temporality of any associations between HIV infection and condom use, and more accurately highlight areas for programmatic focus.
Our study was limited by several factors. About 20% of eligible residents were either not present or declined to participate in the interview and blood draw. Although we do not expect that there is significant participation bias, we were not able to conduct these analyses; however, appropriate weighting was applied to adjust for non-response. These results cannot be generalized to all Kenyans, but only to those that reported recent sexual activity. Additionally, key sexual behavior indicators were based on self reported data. Though KAIS interviewers were trained on asking sensitive questions around sexual behavior and ensuring respondent confidentiality, there is a possibility that these questions were not accurately answered. We did not ask how long after circumcision the men engaged in sexual intercourse. The cross-sectional design of the study limited our interpretation of the temporality of association between the factors examined and HIV infection. The survey also did not ask questions on men having sex with men or injecting drug use activities that are practiced in Kenya and may contribute to new HIV infections [13]. We did not include children due to the relatively low HIV prevalence among this group.
HIV remains a major public health challenge in Kenya. Although various prevention, care and treatment programs have been initiated and expanded in Kenya, evidence based prevention efforts that target known behavioral and biologic factors such as reduction of sex partners, condom use, delayed sexual debut and male circumcision should be enhanced. The wide regional variation in HIV prevalence reinforces the need for targeted prevention interventions focusing on provinces with high infection rates, while at the same time addressing the key behavioral factors that are associated with the risk of HIV infection nationally.
ACKNOWLEDGEMENTS
Special thanks to Professor George Rutherford of the University of California, San Francisco, for his useful comments and assistance in editing this paper
Supported by the U.S. President’s Emergency Plan for AIDS Relief, through CDC/HHS and USAID.
CONFLICTS OF INTEREST
None declared.
DISCLAIMER
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.


