All published articles of this journal are available on ScienceDirect.
The Roles of Youth in Intimate Partner Relationships and the Perceived Risk of HIV Infection in South Africa
Abstract
Background:
Young people in South Africa face multiple developmental challenges, including violence and HIV infection.
Objective:
This study examines the various roles of youth in violent intimate relationships (IPV) and its association with the perceived risk of HIV infection. Results from this study could assist in youth development programmes to increase HIV testing, as well as inform modifications to the South African Domestic Violence Act (No. 116 of 1998), which addresses all forms of intimate partner violence in the country.
Methods:
The study uses data from the South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey (SABSSM) 2017. The study population is youth (15-24 years old) who responded to a question on their perceived risk of being infected with HIV. A weighted sample (N) of 1,301,550 youth is included. The main independent variable is the 'role in IPV', and the study controls for the demographic, socioeconomic, and HIV knowledge and sexual behaviours of youth. Cross-tabulations and a multivariate binary logistic regression model are used to determine the relationship between controls and the outcome.
Results:
About 20% of youth perceive themselves at risk of being with HIV. Their reasons for believing this are because they are sexually active, do not use condoms consistently, and do not trust their partners. Only about 4% of IPV perpetrators, compared to 23.71% of victims and 23.16% of bidirectional youth, think it is likely they will get infected with HIV. The odds of perceiving themselves at risk are higher (with p-values<0.05) for victims (OR=1.21), 20-24 years old (OR=1.35), female (OR=1.25), those who responded do not think condoms reduce the risk of HIV (OR=1.49) and those who do not use condoms (OR=1.44) among others.
Conclusion:
IPV behaviours are associated with perceived HIV risk among young people in South Africa. For perception to change and allow youth to adopt protective behaviours against HIV, there is a need for policy to target the different roles of youth.
1. INTRODUCTION
The HIV and AIDS epidemic in South Africa continues to be a major public health concern. For decades, researchers, health practitioners, and the government have grappled with trying to reduce infection rates and increase the quality of life for people living with HIV. Some successes have been made in the areas of preventing mother-to-child transmissions and the rollout of antiretroviral treatments (ARVs) to previously disadvantaged populations [1, 2]. However, rates of infection remain stubbornly high at almost 14% of the population being infected [3]. Of particular concern are the rates among young people (15-24 years old) that have declined in prevalence by only about 1% in the last 20 years [3]. The current youth prevalence rate of HIV in South Africa is approximately 5.79% [3].
The adoption of HIV prevention behaviours remains key to reducing incident rates in South Africa and other highly affected countries. However, adopting these behaviours is contingent on many factors, including one’s perceived risk of contracting HIV. For young people, the ability to protect themselves from HIV infection is hampered by poverty and inequality, which results in risky sexual practices, including non-condom use in different circumstances [4, 5]. Research has shown that young people who are in relationships of domestic violence are less likely to use condoms and test for HIV than youth who are not in these relationships [6]. Further, in South Africa, gender-based violence is high, with rates of between 12% and 28% of females having ever experienced rape in their lifetime [7]. For adolescents and young females, the rates of violence, including physical and sexual assault from an intimate partner, are high at about 13% [8]. Violence from intimate partners makes safe sex practices difficult for young people to negotiate out of fear of further or more aggressive violence, with research showing females in abusive relationships are particularly reluctant to use pre-exposure prophylaxis (PReP) because they anticipate it will trigger more violence from their male partners [9].
However, young people are not only the victims in violent relationships; they are also perpetrators and, in some relationships, are both the victim and the perpetrator. Perpetration of violence against an intimate partner could be the result of having witnessed violence at young ages between parents and caregivers or being assaulted and abused by parents and caregivers [10]. The latter role of being both the victim and perpetrator in a relationship has been referred to as ‘bidirectional’ intimate partner violence, and in this case, either both partners are violent and abusive, or a partner who was a victim in a previous relationship is now a perpetrator, or vice versa [11-17].
The perceived risk of HIV by role in intimate partner violence is less known [18, 19]. To fully understand risk susceptibility among young people, all aspects and roles of involvement in intimate partner violence need to be examined. This is even more important in a country like South Africa, where both intimate partner violence and HIV rates are high among youth. An investigation into the possible relationship between these concurrent challenges needs to be fully unpacked and more thoroughly studied. Therefore, this study aims to determine the association between the different roles of partners within violent intimate relationships and the perceived risk of HIV infection among youth (15-24 years old) in South Africa.
2. MATERIALS AND METHODS
2.1. Data
This cross-sectional study is set in South Africa and uses data from the South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey (SABSSM) 2017 data, which is a nationally representative survey conducted by the South African Human Sciences Research Council (HSRC) [20]. The data set has modules that contain information on biographical data, school attendance, knowledge, attitudes, beliefs, and values about HIV/AIDS, sexual history, sexually transmitted infections, HIV testing and risk perception, and violence in relationships, among others. Since these data are freely downloadable for research, there was no need to obtain ethics approval. None of the authors were involved in the data collection, and a request to access the anonymised data was obtained from the HSRC in 2019.
2.2. Study Population
The population of interest in this study is youth aged 15-24 years old. The study excludes any youth who did not respond to the question on ‘perceived HIV risk’ (missing cases: 14.15%, n= 1,718; N= 864,474) and those who responded as being HIV positive (0.12%, n=9; N=11, 630). The study also excluded youth who responded ‘no’ to the question “Have you ever been in a relationship?” (7.53%, n=106, N=83,490). Thus, a weighted sample (N) of 1,301,550 (n=1,299) youth are included in the study.
2.3. Study Variables
The dependent variable of the study is ‘perceived HIV risk’ and is measured using the survey question, “On a scale of 1 to 4 (with 1 being low and 4 being high), how would you rate yourself in terms of risk of becoming infected with HIV?”. For this study, responses of “definitely going to get infected” (N=42,638, 3.28%) and “probably will get infected” (N=219,749, 16.88%) are grouped together as ‘will get infected’. While the responses “definitely will not get infected” (N=573,707, 440.8%) and “probably won’t get infected” (N=465,455, 35.76%) are grouped together as ‘will not get infected’. Of particular interest to this study are those who feel they ‘will get infected’ (N= 262,387, 20.16%).
The study also analyses the various reasons youth respondents gave for feeling they will or will not get infected. These are taken from two separate questions on the survey where specific lists of reasons were offered, and respondents could choose one. An ‘other’ option is offered but with no follow-up for an open-ended response. Because of this, the ‘other’ reasons are not analysed in any detail in this study.
The main independent variable is the ‘intimate partner violence role’ and is measured by combining the responses to two questions in the survey. First, respondents were asked, “Did your partner ever do any of the following things to you that could hurt you?”. There is a list of 11 possible types of violence, including being slapped, hit, pushed, punched, and forced to have sex, among others. Respondents who answered “yes” to any one of these items were coded as ‘victims’ in this variable. Second, the survey asked respondents, “Have you ever hit, slapped, kicked, or done anything else to hurt your partner physically?” and those who responded “yes” were coded as ‘perpetrators’ in this variable. The remaining categories in this variable were ‘no violence’ for those who are neither victims nor perpetrators and ‘bidirectional’ for those who have experienced violence (‘victims’) and who have perpetrated violence against a partner.
There are a number of control variables in the study, including the respondents' demographic and socioeconomic characteristics. The demographic variables include age (15-19 years old or 20-24 years old), sex (male or female), race1 (African, White, Coloured, Indian/Asian, Other), marital status (married, never married, previously married) and disability status (yes or no). The socioeconomic characteristics are the highest level of completed education (still in school, primary, secondary, tertiary, never been to school) and employment status (unemployed/student, employed). The study also includes confounding variables. The first two relate to HIV knowledge and are “Can AIDS be cured?” and “Can a person reduce the risk of HIV by using a condom every time he/she has sex?” both have ‘yes’, ‘no’ or ‘don’t know’ responses. The second set of confounding variables relate to sexual activity and are: ‘age at sexual debut’ (arranged around the mean age of 17 years old), ‘condom use at last sex’ (yes or no), and “ever had an HIV test” (yes or no). These confounders are included as research shows all of these to have an impact on perceived HIV risk but are also related to intimate partner violence [21-23].
2.4. Data Analysis
To describe the study population by the outcome of perceived HIV risk, cross-tabulations and chi-square to assess statistical significance (p-values) were used. Further, ranking reasons for perceived HIV risk was done using sorted tabulations. Finally, an adjusted multivariate logistic regression showing odds ratios was used to show the likelihood that respondents would perceive their HIV risk as likely by all characteristics of the respondents.
3. RESULTS
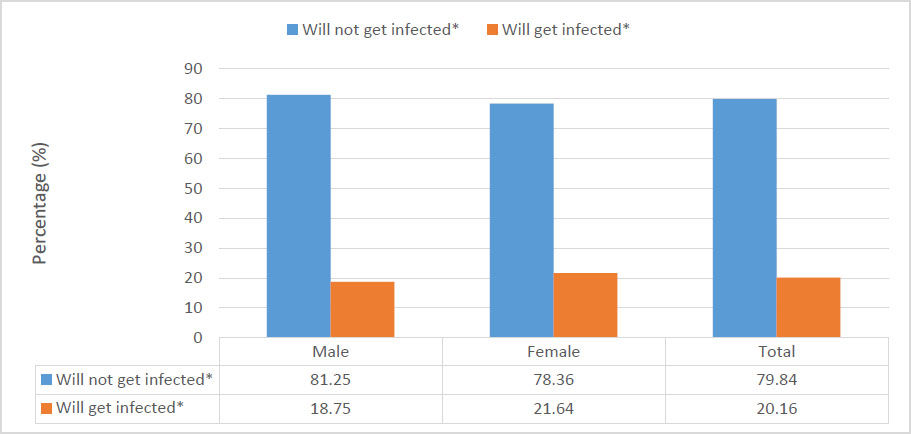
Fig. (1) shows the percentage distribution of sex of the respondents by their perceived likelihood of being infected with HIV. Among males, 18.75% and 21.64% of females believe they will get infected. Overall, 20.16% of youth respondents perceive themselves as ‘will get infected’ with HIV.
Table 1 shows the ranked reasons for perceived HIV infection by sex of the respondents. Based on the number of responses for each perception by sex and for both, the authors ranked the most commonly cited perceptions. Among those who feel they will not get HIV, using condoms is the highest ranked (1) reason for both males and females, followed by being faithful to their partner (2), trusting their partner (3), and abstaining from sexual intercourse (4). Among those who feel they will get HIV, there is less consistency in ranking reasons between male and female respondents. For females, being sexually active is ranked the highest (1) but for males not always using condoms is ranked first. For males, being sexually active is ranked second, while for females, not always using condoms is second. Not using a condom is ranked third (3) for female respondents but fourth (4) for males. Finally, not trusting a partner is third (3) for males but fourth (4) for females. These ranking differences continue for all items on the list.
| Reasons for Perceived HIV Risk | Rank | Frequency (N) | Percentage (%) | ||
|---|---|---|---|---|---|
| Will not get HIV | Male | Female | Both | Both | Both |
| Total | - | - | - | 1 012 630 | 100 |
| Use condoms | 1 | 1 | 1 | 363 908 | 35.94 |
| Faithful to partner | 2 | 2 | 2 | 178 766 | 17.65 |
| Trust partner | 3 | 3 | 3 | 120 268 | 11.88 |
| Abstain | 4 | 4 | 4 | 112 100 | 11.07 |
| Not at risk for HIV | 5 | 8 | 5 | 56 186 | 5.55 |
| Knows partner status | 7 | 5 | 6 | 55 474 | 5.48 |
| Never had sex | 6 | 7 | 7 | 51 164 | 5.05 |
| Knows status | 8 | 6 | 8 | 50 428 | 4.98 |
| No sex workers | 9 | 0 | 9 | 19 118 | 1.89 |
| God protects | 10 | 9 | 10 | 5 006 | 0.49 |
| Ancestors protect | 0 | 10 | 11 | 213 | 0.02 |
| Will get HIV | - | - | - | - | - |
| Total | - | - | - | 242 435 | 100 |
| Sexually active | 1 | 2 | 1 | 79 286 | 32.7 |
| Not always condoms | 3 | 1 | 2 | 63 274 | 26.1 |
| No condoms | 2 | 4 | 3 | 49 886 | 20.58 |
| Don’t trust partner | 6 | 3 | 4 | 25 381 | 10.47 |
| Many partners | 4 | 6 | 5 | 12 865 | 5.31 |
| Accident/cut | 5 | 5 | 6 | 10 621 | 4.38 |
| Partner is sick | 7 | 7 | 7 | 1 121 | 0.46 |
Fig. (2) shows the percentage distribution of sex by intimate partner violence role among youth respondents. More males experience no violence at 53.77% compared to females at 46.23%. Further, 68.75% of the victims of violence are female compared to 31.25% which are males. Almost 52% of those who admitted to hitting a partner (perpetrator) are female, compared to 48.13% of males. About 53% of those who are bidirectional, compared to 47.01% of females. About 80% of both sexes (male and female respondents) did not experience violence, while 10.95% were victims, 2.365 were perpetrators, and 6.17% were identified as engaging in bidirectional violence.
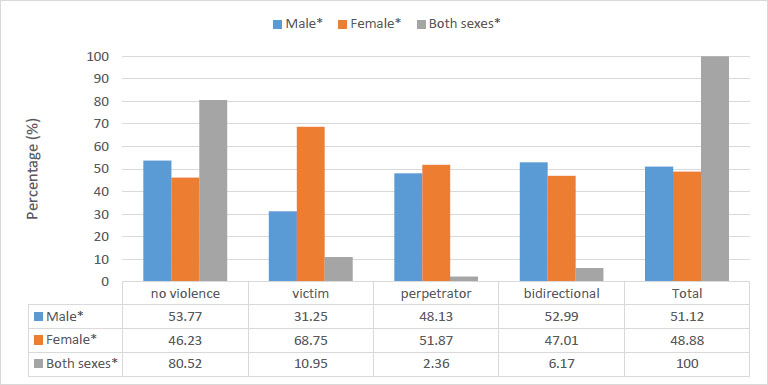
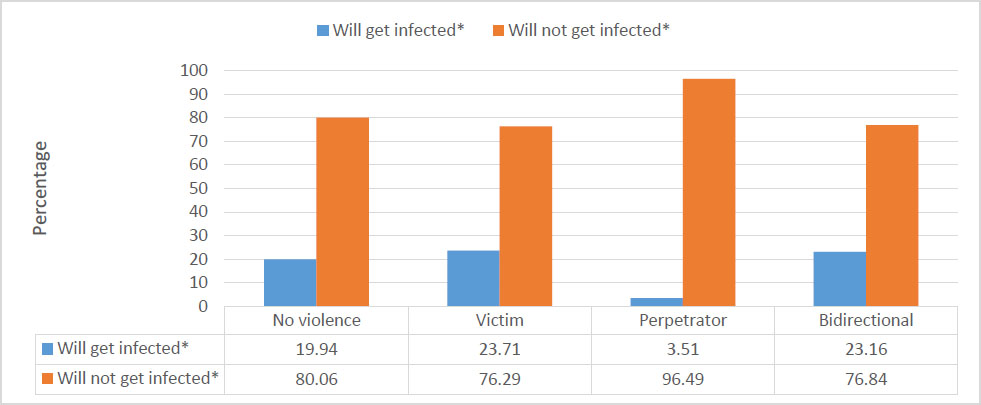
Fig. (3) shows the percentage distribution of perceived HIV risk by the role of the respondent with regard to role in intimate partner violence. For those who have not experienced any violence, 19.94% of youth think they will be infected with HIV. Among the victims, 23.71% perceive themselves as ‘will get infected’, compared to 76.29% who ‘will not get infected’. For perpetrators of intimate partner violence, 3.51% ‘will get infected’ with HIV, and among youth who are bidirectional, 23.16% believe that they will get HIV.
Table 2 shows the frequency and percentage distribution of youth respondents’ characteristics by perceived HIV risk. The overall demographic characteristics of the youth included in the sample are mostly 20-24-year-olds, predominantly African, never married, and with no reported disability. Among younger youth, 15-19 years old, 17.09% and 21.35% of 20-24-year-olds perceived themselves as ‘will get infected’ with HIV. By race or population group, among Africans, the perceived risk of being infected with HIV is 21.94% compared to 11.26% among Whites, 3.95% among Coloured, and 9.92% among Indian/ Asian youth. Almost 21% (20.54%) of never-married and 10.74% of married respondents think they will get HIV. Among youth with a reported disability, 63.43% believe they will get HIV. For youth who are still in school, 16.74%, those with a primary education, 19.08%, and for youth with a secondary education, 24.30% ‘will get infected’ with HIV. Among the respondents who are unemployed or still students, 21.72% perceive their HIV risk as likely. By HIV knowledge indicators, respondents who believe there is a cure for HIV or did not know the correct answer, 20.84% perceivably will get infected with HIV. Further, 25.12% of respondents who do not believe that condoms reduce the risk of infection also believe that they are likely to be infected with HIV. By sexual behaviour indicators, 23.75% of those youth whose age at first sex was younger than 17 years old (or the mean age of the sample) believe they will be infected as well as 29.30% of those who did not use a condom at last sex and 16.73% of those who have never tested for HIV.
| Respondent Characteristics | Perceived HIV Risk | ||||
|---|---|---|---|---|---|
| Will not get Infected | Will get Infected | Total | |||
| N | % | N | % | N | |
| Total | 1 039 163 | 79.84 | 262 387 | 20.16 | 1 301 550 |
| Age group* | - | - | - | - | - |
| 15-19 | 300 460 | 82.91 | 61 921 | 17.09 | 362 381 |
| 20-24 | 738 703 | 78.65 | 200 466 | 21.35 | 939 169 |
| Race* | - | - | - | - | - |
| African | 859 453 | 78.06 | 241 595 | 21.94 | 1 101 048 |
| White | 80 119 | 88.74 | 10 166 | 11.26 | 90 285 |
| Coloured | 18 890 | 96.05 | 777 | 3.95 | 19 667 |
| Indian/Asian | 60 456 | 90.08 | 6 655 | 9.92 | 67 111 |
| Marital Status* | - | - | - | - | - |
| Married | 37 948 | 89.26 | 4 568 | 10.74 | 42 516 |
| Never Married | 997 467 | 79.46 | 257 819 | 20.54 | 1 255 286 |
| Previously Married | 3 748 | 100.00 | 0 | 0.00 | 3 748 |
| Disability Status* | - | - | - | - | - |
| Yes | 3 365 | 36.57 | 5 837 | 63.43 | 9 202 |
| No | 1 035 797 | 80.15 | 256 550 | 19.85 | 1 292 347 |
| Highest level of education* | - | - | - | - | - |
| Still in school | 460 262 | 83.26 | 92 529 | 16.74 | 552 791 |
| Primary | 34 626 | 80.92 | 8 164 | 19.08 | 42 789 |
| Secondary | 471 992 | 75.70 | 151 546 | 24.30 | 623 539 |
| Tertiary | 56 294 | 89.10 | 6 888 | 10.90 | 63 181 |
| Never went to school | 15 989 | 83.06 | 3 260 | 16.94 | 19 249 |
| Employment Status* | - | - | - | - | - |
| Unemployed/student | 832 341 | 78.28 | 230 994 | 21.72 | 1 063 335 |
| Employed | 206 821 | 86.82 | 31 393 | 13.18 | 238 214 |
| There is a cure for HIV* | - | - | - | - | - |
| Yes / don’t know | 221 882 | 79.16 | 58 427 | 20.84 | 280 309 |
| No | 817 281 | 80.03 | 203 960 | 19.97 | 1 021 240 |
| Reduce HIV risk through condom use* | - | - | - | - | - |
| Yes | 915 551 | 80.56 | 220 920 | 19.44 | 1 136 471 |
| No/don’t know | 123 612 | 74.88 | 41 467 | 25.12 | 165 078 |
| Age at first sex* | - | - | - | - | - |
| <17 years old | 404 485 | 76.25 | 125 993 | 23.75 | 530 478 |
| 17+ years old | 528 622 | 81.52 | 119 835 | 18.48 | 648 457 |
| Didn’t answer | 106 056 | 86.49 | 16 559 | 13.51 | 122 615 |
| Condom use at last sex* | - | - | - | - | - |
| Yes | 434 963 | 80.33 | 106 525 | 19.67 | 541 488 |
| No | 119 432 | 70.70 | 49 498 | 29.30 | 168 930 |
| Didn’t answer | 484 768 | 82.01 | 106 364 | 17.99 | 591 131 |
| Ever tested for HIV* | - | - | - | - | - |
| Yes | 759 285 | 78.65 | 206 139 | 21.35 | 965 423 |
| No | 279 878 | 83.27 | 56 248 | 16.73 | 336 126 |
Table 3 presents the odds (likelihood) that the youth respondents would perceive themselves as ‘will get infected’ with HIV. All control variables selected for the study are included in this model. The odds are higher for those respondents who are victims (OR=1.21, p-value<0.05), 20-24 years old (OR=1.35, p-value<0.05), female (OR=1.25, p-value<0.05), never married (OR=2.50, p-value<0.05), those with primary education at most (OR=1.28, p-value<0.05), those with secondary education at most (OR=1.72, p-value<0.05), those who responded do not think condoms reduce the risk of HIV (OR=1.49, p-value<0.05) and those who do not use condoms (OR:1.44, p-value<0.05). The table also shows that the odds of ‘will get infected’ with HIV perception is less for youth who are perpetrators of intimate partner violence (OR=0.15, p-value<0.05), bidirectional (OR=0.96, p-value<0.05), any race or population group other than African (reference category), have no reported disability (OR=0.09, p-value<0.05), are employed (OR=0.58, p-value<0.05), stated there is no cure for HIV (OR=0.877, p-value<0.05), age at first sex was 17 years old or older (OR=0.63, p-value<0.05) and have never tested for HIV (OR=0.94, p-value<0.05).
| Respondents Characteristics | Odds Ratio (OR) | P-value | Confidence | Interval |
|---|---|---|---|---|
| Intimate partner violence role* | - | - | - | - |
| no violence | RC | - | - | - |
| victim | 1.21 | 0.000 | 1.190235 | 1.224748 |
| perpetrator | 0.15 | 0.000 | 0.1435648 | 0.162332 |
| bidirectional | 0.96 | 0.000 | 0.9384425 | 0.972349 |
| Age group* | - | - | - | - |
| 15-19 | RC | - | - | - |
| 20-24 | 1.35 | 0.000 | 1.335996 | 1.368556 |
| Sex* | - | - | - | - |
| Male | RC | - | - | - |
| Female | 1.25 | 0.000 | 1.234581 | 1.259325 |
| Race* | - | - | - | - |
| African | RC | - | - | - |
| White | 0.40 | 0.000 | 0.3909045 | 0.409282 |
| Coloured | 0.20 | 0.000 | 0.1819549 | 0.210348 |
| Indian/Asian | 0.59 | 0.000 | 0.5733894 | 0.605313 |
| Marital Status* | - | - | - | - |
| Married | RC | - | - | - |
| Never Married | 2.50 | 0.000 | 2.424386 | 2.587737 |
| Disability Status* | - | - | - | - |
| Yes | RC | - | - | - |
| No | 0.09 | 0.000 | 0.0875769 | 0.09573 |
| Highest level of education* | - | - | - | - |
| Still in school | RC | - | - | - |
| Primary | 1.28 | 0.000 | 1.244566 | 1.313949 |
| Secondary | 1.72 | 0.000 | 1.701088 | 1.736668 |
| Tertiary | 0.71 | 0.000 | 0.6907287 | 0.729371 |
| Never went to school | 0.96 | 0.029 | 0.9187039 | 0.995336 |
| Employment Status* | - | - | - | - |
| Unemployed/student | RC | - | - | - |
| Employed | 0.58 | 0.000 | 0.5747243 | 0.591113 |
| There is a cure for HIV* | - | - | - | - |
| Yes / don’t know | RC | - | - | - |
| No | 0.87 | 0.000 | 0.8613514 | 0.88031 |
| Reduce HIV risk through condom use* | - | - | - | - |
| Yes | RC | - | - | - |
| No/don’t know | 1.49 | 0.000 | 1.47253 | 1.510843 |
| Age at first sex* | - | - | - | - |
| <17 years old | RC | - | - | - |
| 17+ years old | 0.63 | 0.000 | 0.6209652 | 0.63365 |
| Didn’t answer | 0.68 | 0.000 | 0.6705122 | 0.697282 |
| Condom use at last sex* | - | - | - | - |
| Yes | RC | - | - | - |
| No | 1.44 | 0.000 | 1.421744 | 1.459438 |
| Didn’t answer | 1.01 | 0.018 | 1.002205 | 1.023501 |
| Ever tested for HIV* | - | - | - | - |
| Yes | RC | - | - | - |
| No | 0.94 | 0.000 | 0.9270181 | 0.9482 |
4. DISCUSSION
The purpose of this study was to determine if a relationship exists between intimate partner violence roles and perceived HIV risk among youth in South Africa. This study is needed because the HIV prevalence among youth in the country is high, and without more effort into understanding the various dynamics affecting the perceived risk of infection, prevention behaviours will not be fully adopted.
The main finding of the study is that intimate partner violence roles, to varying degrees, play a part in how youth perceive their risk of contracting HIV. Victims have the highest likelihood and prevalence of believing that they will get HIV. This is similar to other studies that argue the diminished agency, which includes the inability to control their actions and lives, that abused partners feel makes it difficult to discuss and practice safe sex with violent partners [24, 25]. Therefore, their heightened belief to be at risk of HIV infection is plausible. This study, however, showed that perpetrators, while having a lower likelihood of perceived HIV susceptibility, still believe they will get infected with the virus. This may not be related to violence and could be the result of other unsafe sexual practices, including lack of condom use. Not trusting their intimate partner has been cited as a cause for violence by perpetrators and could also suggest a reason for believing that they will get infected with HIV [26, 27]. In the case of respondents who are bidirectional, almost a quarter believe it is likely they will be infected with HIV. Since these youth are both victims who are unable to negotiate safe sex and perpetrators who may suspect partners of infidelity, it is a warranted result that they feel more certain of being infected. For young people to become bidirectional in violent relationships, research suggests that gendered differences in the risk factors exist. For young males, experiences of childhood sexual abuse and neglect are attributed to later perpetration and experiences of violence from a partner, while for young females, childhood neglect and low self-esteem are found to cause perpetration and victimisation [28].
The sex differences found in this study are quite striking in terms of intimate partner violence role, perceived risk of HIV infection and the ranked reasons for risk perception. To begin, the study found a significant number of females reported being perpetrators of violence. Very little research is done on female perpetrators, but what is known is that it is caused by, among other things, substance use, traumatic experiences, emotional regulation difficulties, and poor mental health outcomes [29]. It could also be self-defence; however, the act of physically hurting a partner, as defined by the survey question in this study, does not differentiate between self-defence and the perpetration of violence when not in physical danger. More research on females acting in self- defence in a violent relationship has been done, and it shows that females are more likely to be violent in relationships due to the need to self-protect or because of poor conflict management within aggressive relationships; however, jealousy and anger were also found to be contributing factors [30-33].
More young females than young males also believe they will be infected with HIV because they are sexually active and do not always use condoms, in that order of ranking. Females having a more heightened sense of risk could be attributed to having more knowledge of the disease than their male counterparts. Research has shown that young females in South Africa have higher rates of accurate HIV knowledge, with 60.3% having at least core or basic knowledge of the disease [34]. According to the much-used Health Belief Model, knowing the causes, determinants, and prevention means of disease is directly associated with the perceived risk of contracting the disease [35]. This is coupled with their actual sexual behaviours whereby if they are engaging in risky sexual acts, such as inconsistent condom use and having mistrust with their partner (both ranked highly in this study), there is a more likely belief that they are at risk of infection. For young males in the study, the predominant reason for believing they are at risk of HIV infection is inconsistent condom use. Other highly ranked reasons for young males include not trusting their partners and having many sexual partners. This shows that a level of HIV knowledge and awareness among males is accurate in their assessment of risk and is substantiated by other research that found similar results [36-38].
With regard to HIV risk perception, the study found a few interesting demographic and socioeconomic associations. Youth who are reportedly disabled believe they will get infected with HIV. Youth with disabilities report higher rates of sexual assault (odds ratio of 2.27) and are vulnerable to intimate partner violence (odds ratio of 1.17), both of which increase the risk of HIV infection [39, 40]. Research has shown that young people with disabilities do not have accurate knowledge of HIV and AIDS, with one study showing that 88% of respondents with disabilities have poor knowledge [41]. Therefore, insufficient knowledge coupled with the vulnerability of having a disability could explain why youth with disabilities perceive themselves as at risk of infection.
The study further affirms that education and employment are associated with a reduced likelihood of perceived HIV infection. This is not new, as many studies have found that higher education and independent means of earning income place young people in a better position to adopt preventative behaviours and thus have the perception that they will not be infected with HIV [21, 42, 43]. Education and employment, therefore, remain key to reducing young people’s vulnerability to infection. However, in South Africa, where school completion is low in rural areas and public non-fee paying schools, and youth unemployment at 64.16% is high, continued efforts by the government and private sector to prioritise youth development to reduce HIV infections must persist [44, 45].
As mentioned before, a core understanding of the Health Belief Model is that knowledge of disease impacts the behaviours taken to prevent or treat a disease [46, 47]. This study included HIV knowledge variables and found that not having inaccurate knowledge is associated with an increased likelihood of perceiving that they will get HIV. In addition, not adopting risky sexual behaviours such as older age at sexual debut also lowers the odds of a likely perception of getting HIV. These proxy measures further substantiate the usefulness of health theories in understanding negative outcomes. However, theories, such as the Health Belief Model, were developed decades ago based on empirical evidence of the time. Since then, this model has been adapted to apply to non-communicable and other infectious diseases [48, 49]. Sadly, after decades of research using this model to understand HIV and AIDS, there is little evidence, as suggested by the current study, that anything is changing. That is, behaviours are not changing, making the application of this model still relevant but with little progress toward meeting the end goal of HIV reduction.
The study is subject to a few limitations. First, further investigation into the ‘other’ reasons respondents gave for believing they are or are not at risk of HIV could not be done. While this is an option on the survey, there is no follow-up for open-ended responses. This could have informed future survey designs and research on additional and perhaps more relevant reasons among youth in contemporary South Africa and similar countries. Second, the question of the perpetration of violence does not specify whether this was self-defence. This would inform risk perception in more detail. Similarly, the survey is cross-sectional; therefore, it is impossible to determine if the victimisation and perpetration of violence in intimate partner relationships are concurrent or referring to subsequent relationships. It is becoming increasingly important that concurrent bidirectional violent relationships are investigated because the dynamics within these relationships are less known in relation to health outcomes, including HIV risk perception.
CONCLUSION
Behaviour change is key to reducing likely perceptions of HIV infection among youth in South Africa. Key demographic and behavioural factors have been identified in this study, including females, lower levels of education, never married, knowledge of condoms to reduce HIV transmission, and using condoms, which are all associated with perceived risk of infection. In addition, intimate partner violence is related to an increased perception of HIV risk among youth. Efforts to reduce intimate partner violence must be taken more seriously, as supported in the country’s Domestic Violence Act (No. 116 of 1998) and address all parties and directions of violence (victims, perpetrators, and bidirectional) in order to change young people’s perceptions of risk and ultimately enable them to adopt more preventative behaviours. Future studies should focus on the vulnerable identified in this study which include youth with disabilities, those who are both victims and perpetrators of violence, and youth affected by under-education and unemployment in qualitative study designs to understand how and why these are risk factors for likely perceptions of HIV infection.
LIST OF ABBREVIATIONS
| IPV | = Intimate Relationships |
| ARVs | = Antiretroviral Treatments |
| PReP | = Pre-exposure Prophylaxis |
| HSRC | = Human Sciences Research Council |
| OR | = Odds Ratio |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study uses secondary data, which none of the authors assisted in collecting. The Human Sciences Research Council of South Africa obtained ethics approval from the HSRC Research Ethics Committee (REC: 4/18/11/15), the CDC Division of Global HIV and TB (DGHT), and the CDC’s Center for Global Health (CGH).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data used in this study are freely available for download from https://repository.hsrc.ac.za/handle/20.500. 11910/15468
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
The Demography and Population Studies Department at the University of the Witwatersrand.


