All published articles of this journal are available on ScienceDirect.
HIV and Risk Behaviors Among Visitors of Inmates at the Great Tehran Prison, Iran, 2018
Abstract
Objectives:
The objective of the present study was to determine the prevalence of HIV and risk behaviors among the inmates’ visitors at the Great Tehran Prison in 2018.This population is more likely to be infected with HIV due to their relationship with inmates. However, they have not been prioritized to the other populations in comparison to inmates who are usually prioritized over others.
Methods:
Using a time location sampling (TLS) bio-behavioral survey, we recruited inmates’ visitors at the Great Tehran Prison in 2018. An anonymous questionnaire collected information on the participant’s demographic characteristics, relationship with inmate, imprisonment history, drug-related risk behaviors, and HIV-related risk behaviors.Rapid HIV blood test detected HIV positive people. To examine the association between risk behaviors and HIV infection, we used a multivariate logistic regression model to calculate the adjusted Odds Ratio (OR)(adjusted Odds ratio of 23.140, 95% CI OR: 1.994–268.5).1
Results:
1131 visitors were asked to participate in the study; out of which 1120 consented (99%).Out of the 1120 participants, 55.2% were female, and the majority (72.4%) aged older than 35 years. Of those who had a sexual partner, 50% did not usea condom in the last 6 months. Overall, HIV prevalence was 0.4% in the inmate visitors, but it was significantly higher among those with a history of drug injection(p=0.003).
Conclusion:
Our findings indicated that overall the HIV prevalence is low among inmates’ visitors; higher than general population. Subgroups with a history of injection have high HIV prevalence which needs to be prioritized for HIV screening and treatment.
1. INTRODUCTION
There are about 230,000 inmates in Iran [1]. The prevalence of HIV among inmates is higher than the general population [2, 3] which attributed to the low socioeconomic condition, lack of knowledge about HIV and its transmission routes, drug injection, high-risk sexual behaviors, and tattoos in inmates [4-6]. Prisons and other temporary residential facilities (such as camps and shelters) have reported having a higher rate of HIV transmission [7, 8].
Imprisonment not only increases the risk of HIV transmission among the incarcerated populations but also it is likely the risk to be higher among other members of society through unsafe sexual or drug practices [9]. Given the short average time of being in prison (about 6 months)2 and the risk of acquiring HIV infection within the prison and then transmitting to others upon release, most of the HIV programs have included inmates people as a priority population [9]. One study documented that 50% of Hispanic inmates had sex within the first 12 hours after release from prison [10]. The majority of men in relationships had unprotected intercourse with their primary partners within days of paroling from prison [11].These findings indicated a high potential risk of HIV transmission to inmates’ sexual partners.According to a study in Iran, turnover of prisoners back to society is high and while prisoners are not separated in prison based on the history of drug use, they might transmit the HIV within the prison which in turn can amplify the possibility of transmitting infection outside of the prison to inmates’ sexual partners or people in their drug use circle [4].
Inmates who used to inject or use drugs still have fair access to drugs inside the prisons [12], and of course, upon release, they most likely continue to drug use, share injection kits, and even overdose [13].This puts their family members who also use drugs at risk for HIV infection.
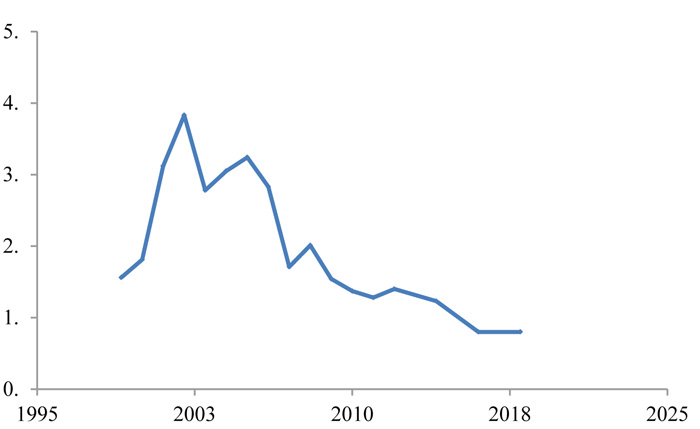
Besides the potential higher risk for HIV infection among inmates’ visitors, this group has not been studied very well. As the rate of HIV infection among inmates is higher than in society (Fig. 1), this study was designed to investigate the prevalence of HIV infection among inmates’ visitors who may be exposed to HIV infection more than other people. Moreover, investigation of related risk factors was another objective of the present study which helps to reduce the HIV infection risk among this population.
2. METHODS
In this cross-sectional study, we measured the demographic characteristics, HIV prevalence, and HIV-related risk behaviors in 1131 visitors-from which 1120 accepted to participate-of male inmates at the Great Tehran Prison. The participants were recruited using a time location sampling (TLS) bio-behavioral survey and interviewed after collecting informed written consent.
The questionnaire included sections on demographic characteristics, the relationship with inmates, imprisonment history, drug injection-related risk behaviors, and HIV-related risk behaviors. Counseling was also provided regarding HIV transmission and prevention measures and the introduction of HIV testing and counseling services. This was done by two trained researchers in the prison’s visiting room.Those who provided consent for HIV testing were tested by a rapid HIV blood test kit, and if the test results were reactive, they were tested on a second rapid test.Those who were reactive for both rapid tests were considered to be HIV positive.
HIV point prevalence was calculated as the number of HIV-positive individuals divided by the number of test results overall and stratified by demographic characteristics, incarceration history, and drug-use practices.
The data was analyzed using the SPSS software version 22.Variables associated with HIV infection in bivariate analysis at the p ≤ 0.10 levels were included as potential independent predictors. The final model retained those variables associated with HIV infection at the p<0.05 level.
2.1. Ethical Considerations
The protocol of the study was reviewed and approved by the Institutional Review Board (IRB) of Tehran University of Medical Sciences. All the participants were informed and familiarized with the study objectives and methods. The participants were assured about their information anonymity and confidentiality. Informed written consent was obtained from all the participants prior to the study.
3. RESULTS
Out of the 1120 participants, majority were female (55.2%), aged older than 35 years (72.4%), married (83.1%), and first degree family member (i.e. spouse, daughter, sister, mother) (Tables 1 and 2).
Table1.
| Variable | N* (%) | HIV prevalence, N (%) |
|---|---|---|
| Gender | ||
| Male | 618 (55.2) | 2 (0.4) |
| Female | 502 (44.8) | 2 (0.3) |
| Age group | ||
| 35-26 | (27.6)309 | 1 (0.3) |
| 45-36 | (25.9)290 | 2 (0.7) |
| 59-46 | (26.3)295 | 1 (0.3) |
| 60> | (8.5)95 | 0 (0.0) |
| Marital status | ||
| Single | (12.6)73 | 3 (4.1) |
| Married | (83.1)482 | 0 (0.0) |
| Divorced | (3.4)20 | 1 (5.0) |
| Widowed | (0.9)5 | 0 (0.0) |
| Education level | ||
| Illiterate | (16.7)97 | 1 (1.0) |
| Primary school | (15.5)90 | 0 (0.0) |
| Did not complete high school | (23.3)135 | 1 (0.3) |
| Completed high school | (30.2)175 | 0 (0.0) |
| More than high school | (14.3)83 | 0 (0.0) |
| Who you are visiting today? | ||
| Spouse | (25.4)285 | 1 (0.3) |
| Son | 347 (31.0) | 0 (0.0) |
| Brother | 319 (28.5) | 0 (0.0) |
| Father | 47 (4.2) | 1 (2.1) |
| Grandchild | 7 (0.6) | 0 (0.0) |
| Friend | (5.3)59 | 2 (3.4) |
| Other relatives | 40 (3.6) | 0 (0.0) |
| Client | (1.4)16 | 0 (0.0) |
The most prevalent high-risk behaviors among participants were unprotected sex (47.9%), history of addiction (17.6%), marriage to a person with at least one risk factor (16.4%), having multiple partners (14.2%) and history of incarceration (11.2%) (Table 3).
Overall, 4 (0.4%) were HIV positive. HIV prevalence was significantly higher among those with a history of drug injection than others (p=0.003). In multivariate analysis, a history of injection remained independently associated with HIV infection (adjusted Odds ratio of 23,140, 95% CI OR: 1,994-268,5).p =0.003).
4. DISCUSSION
To the best of our knowledge, this study was the first study to assess the HIV prevalence and risk behaviors of inmates’ visitors in Iran. Our findings indicated that overall the HIV prevalence is low among inmates’ visitors; however, those with a history of injection have the highest HIV prevalence which needs to be prioritized for HIV screening and treatment.
Unsafe sex is high among partners of inmates. Female partners of male inmates reported having a good knowledge about HIV and its transmission routes; however, they did not use condoms in sex with their partners when they were released from the prison as they thought they did not have sex or other risk behaviors during incarceration. This is not true as the majority of male inmates had a history of injection and 20% had a second partner [14].We also found that half of the inmates’ visitors did not use condoms during the last 6 months and about three percent reported a history of drug injection.
Table 2.
| Variable | Mean | Std. Deviation | Range |
|---|---|---|---|
| Age | 40.31 | 12.851 | 67 |
| Variables | N (%) | HIV prevalence, N (%) |
|---|---|---|
| Reported history of incarceration* | (11.2)125 | 2 (1.6) |
| Reported history of addiction | (17.6)197 | 2 (1.0) |
| Reported history of injection** | (2.4)27 | 2 (7.4) |
| Reported ever sharing needles or equipment | (0.7)8 | 0 (0.0) |
| Reported ever having unprotected sex | (47.9)537 | 3 (0.5) |
| Reported having multiple partners*** | (14.2)159 | 2 (1.2) |
| Reported history of male-male sex | (1.2)13 | 0 (0.0) |
| Receiving blood and blood products | (0.3)3 | 0 (0.0) |
| Reported history of STD | (7.3)82 | 1 (1.2) |
| Married to a person with at least one risk factor1 | (16.4)184 | 1 (0.5) |
| Reported ever having unprotected sex with HIV+ partner | (0.1)1 | 0 (0.0) |
| Reported having occupational or non-occupational exposure | (0.1)1 | 0 (0.0) |
| History of tattooing | 22 (2) | 0 (0.0) |
| Condom use during last 6 months | ||
| Always | (6.3) 19 | 0 (0.0) |
| Sometimes | (25.7) 77 | 0 (0.0) |
| Rarely | (18) 54 | 0 (0.0) |
| Never | (50) 150 | 2 (1.3) |
| Routes of administration in drug users | ||
| Smoking | (10.9) 122 | 1 (0.8) |
| Oral consumption | (2.3) 26 | 0 (0.0) |
| Injection | (0.3) 3 | 0 (0.0) |
| Smoking/ Oral | (0.5) 6 | 0 (0.0) |
| Oral/ Injection | (0.1) 1 | 0 (0.0) |
| All | (0.3) 3 | 0 (0.0) |
Among women visiting their incarcerated partners at several prisons in California, the HIV prevalence was 1.23%; Factors associated with HIV prevalence were age, incarceration period, history of drug injection, history of needle sharing, and tattooing [15].While HIV prevalence was lower in our study, (i.e. 0.4%), we also found that history of drug injection is the main predictor for HIV.Similar to findings in our study, other concerning risk factors include lack of practical knowledge and positive attitudes toward HIV prevention practices and high frequency of unprotected sex (Table 2 and Table 3) [16].
Male inmates have a high frequency of risk behaviors (unsafe sex or injection), before and after incarceration. Unprotected sex was reported by 46% of the prisoners for the time prior to incarceration, and by 18% at one month and by 24% at three months post-release [17].
Partners of male inmates are at risk for other mental health problems like anxiety and depression which may lead to lower self-esteem and also misjudgment about risk behaviors and risk perception [15]. Having multiple partnerships among partners of male inmates and higher risk rates of STDs and HIV infectionwere reported in the past [18-21]. Women with multiple partnerships reported more history of STDs treatment than those who were in a one-one relationship (26% vs. 11%) [22]. This also explains the slightly higher HIV prevalence among our study population.
5. LIMITATION
Our study had three main limitations. First, the number of HIV positive cases was low in our study and so we did not have the power to fully assess the risk factors of HIV infection. Second, the collected risk behaviors were self-reported hence they were likely to be under-reported. And last, we did not study the HIV and risk behaviors of inmates and their visitors together and so were not able to assess the proportion and predictors of unsafe relationships.
CONCLUSION
Despite the limitations, we found the HIV prevalence to be low among the inmates’ visitors, but higher than general population. Overall subgroups with a history of injection had high HIV prevalence which needs to be prioritized for HIV screening and treatment. Being in a prison for a while provides a window opportunity for prevention interventions, family support, and behavioral change in both inmates and their families. However, right now our best option for intervention is to continue our programs of distributing syringes inside and outside of prison. HIV programs in Iran need to use this opportunity to further improve their response to drug-related HIV epidemics in the country.
NOTES
1 It should be noted that according to the latest Spectrum projections, Iran’s HIV population in 2018 stood at 60,760. For more information see: https://www.unaids.org/en/regionscountries/countries/islamicrepublicofiran
2 SeyedAlinaghi SA, Taj L, Mazaheri E, Ahsani-Nasab S, Abedinzadeh N, Mcfarland W, Mohraz M, Mirzazadeh A. HIV in Iran: Epidemiology, Response, Challenges and Way Forward. AIDS. In Press
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethical committee of Tehran University of Medical Sciences, Tehran, Iran, approved the study protocol under reference no. 8923101017.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013
CONSENT FOR PUBLICATION
The participants were recruited using a convenience sampling method and interviewed after collecting informed written consent.
STANDARD FOR REPORTING
STROBE guidelines and methodology were followed to conduct the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available in the Iranian Research Center for HIV/AIDS at https://research.tums.ac.ir/, reference number 8923101017.
FUNDING
This study was supported by Tehran University of Medical Sciences (grant no.8923101017). For this paper, we also received support from the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS), U.S. NIMH, R25MH064712.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors express thanks to all staff in the Great Tehran Prison for their help. For this paper, we also received support from the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS), U.S. NIMH, R25MH064712.


