All published articles of this journal are available on ScienceDirect.
HIV Prevention: The Key to Ending AIDS by 2030
Abstract
There is no viable substitute for re-energizing, funding and supporting culturally attuned, locally staffed HIV advocacy and prevention programmes, especially in resource poor settings. The evidence that such interventions are effective remains compelling; and although the cost implications are not negligible, the medium to long-term outcomes must be regarded not as complementary, but as integral, to biomedical interventions. The success of the anti-retroviral drugs upscale has enabled a noticeable improvement in AIDS related morbidity and mortality in the recent years; yet the underlying dynamics of the epidemic remains undetermined by the rate at which new infections are taking place in relation to the number of AIDS deaths. While the rate of new HIV infections is stabilising in some of the hardest hit countries, it remains far too high and the future cost of maintaining an ever-expanding pool of people reliant on daily drugs for survival is unsustainable. Countries must exercise caution in continuing to focus on treatment as a ‘quick fix’ to end AIDS as a public health concern. HIV is a socially culturally induced crisis and, as such, a variety of measures are needed simultaneously to appeal to different people, groups and circumstances.
INTRODUCTION
There is no viable substitute for re energizing, funding and supporting culturally attuned, locally staffed HIV advocacy and prevention programmes, especially in resource poor settings. The evidence that such interventions are effective remains compelling; [1] and although the cost implications are not negligible, the medium to long term outcomes must be regarded not as complementary, but as integral, to biomedical interventions. The success of the antiretroviral drugs (ARV) upscale has enabled a noticeable improvement in AIDS related morbidity and mortality in the recent years; yet the underlying dynamics of the epidemic remains undetermined by the rate at which new infections are taking place in relation to the number of AIDS deaths - (Fig. 1). Worldwide there are still very few countries that have been able to either reverse the spread of the epidemic on a sustainable basis or stop its progression, and fewer programmes on prevention have been scaled up to a national level.
While the rate of new HIV infections is stabilising in some of the hardest hit countries, it remains far too high and the future cost of maintaining an ever expanding pool of people reliant on daily drugs for survival is unsustainable [2]. In what follows I caution against the wisdom of continuing to focus on treatment as the backbone of the global strategy against HIV and AIDS. I suggest that the pursuit of this 'quick fix' has led to over reliance on biomedical interventions for prevention, displacing something we learned very early in the epidemic’s history - namely, that HIV is a socially culturally induced crisis and, as such, a variety of measures are needed simultaneously to appeal to different people, groups and circumstances. I start my analysis with the challenge facing the HIV and AIDS community as the world heads towards embracing the Sustainable Development Goals (SDGs).
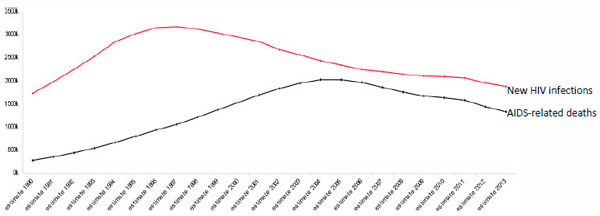
Yearly new HIV infections and AIDS related deaths globally, 1990-2013 [3].
Treatment, an Unsustainable Future
Under its new ‘Fast Track’ strategy, the Joint United Nations Program on HIV and AIDS (UNAIDS), renewed its 2011 commitment to eradicate ‘AIDS as a public health concern by 2030’ [4]. If this ambition is to be realised, then a long over due rethink about what works in HIV prevention and how to successfully scale it up across regional, national and subnational levels, is urgently needed. For all the stunning success of the ART roll out, the single most worrying counter indication is that the number of new HIV infections exceeds the number of people being enrolled on ART programmes [5]. This indicates considerably more than a trend that can be reversed in simple arithmetic terms. This is because the headline numbers mask complex human, logistical and disease dynamics which compound the difficulties of further progress for both prevention and treatment. Clinical complications and treatment failures have a variety of sources including inadequate screening, drug resistance and chronic side effects which affect adherence to drug regimes, exacerbated by breaks in delivery supply chains [6], weak health systems and inadequate monitoring. Moreover, however it is occasioned, ARV drug resistance is transmissible, which further amplifies the disparity between the deterioration of prevention programmes and proposed extensions of ART coverage.
Significant hope has been invested in ART as a preventative, particularly if the programmes can quickly be extended to HIV positive people with higher CD4 counts than those currently eligible. The logic is not as farfetched as it may sound: anti retrovirals function by stopping HIV from spreading in the body. In the recent years, a number of research studies suggest that while someone is taking the ARVs, the virus almost disappears from their blood stream, and importantly, from their seminal fluids. Moreover, in infected female individuals, the drugs have a tendency to accumulate in the tissue of the vagina [7]. So far studies on this in Africa are limited, but work in Taiwan, British Columbia and the United Kingdom indicates significant declines in transmission rates as ARVs have increased over time [7]. More conclusive data is needed, and work is underway in a number of sites across the world [7]. One of the most intriguing is a clinical trial involving ‘discordant’ couples (where one partner is infected with HIV and the other is not), to establish whether ARVs really do reduce transmission. This trial, which is taking place at the University of North Carolina, Chapel Hill, United States, will not report for at least another two years, but the outcomes are hugely anticipated.
More recently the results of a major UK trial of pre exposure prophylaxis (PrEP) have been hailed as ‘extremely exciting’ and a ‘game changer’ by leading scientists. Under the UK trial, some 545 HIV negative gay men, who were sexually active and had recently had unprotected sex, were recruited into the study. The study found that PrEP reduced the risk of infections amongst those on the trial by an unprecedented 86%. Among the 276 men given PrEP immediately after each sexual experience, there were only three HIV infections in the first year of the study, compared to 19 among the deferred group. The British trial was primarily about giving ARVs to HIV negative people, to prevent them from becoming infected in the first place. The success of the British clinical trial raises the ethical question about whether the approach should be extended to all vulnerable or at risk groups. In the UK, it is estimated that the cost of doing so would be around GBP 500 per person per month. The cost of the drug itself (Truvada - which is a combination of two antiretroviral drugs) is estimated at GBP 361 for 30 pills - one month’s provision. On top of that, the estimated price of providing the drug through clinics might costs around GBP 62.50 per month, using provision costs.
‘Based on current [World Health Organisation] recommendations (HIV-positive individuals with CD4 count <350), 21 million people are eligible for ART, yet only 9.7 million are being treated. Expanding coverage to HIV-positive individuals with CD4 counts <500 and children aged <5 years increases eligibility to 26 million people, and universal ‘test and treat’ of all HIV-positive individuals would see 32 million people eligible for treatment’ [8]. With incomplete and/or patchy ART coverage, reports of rationing, breaks in the supply chain and incomplete transitions to newer forms of ART, the challenges facing ART as prevention on the scale required are considerably in excess of what might be captured in the phrase, ‘scaling up’. In any event, ‘data from real life implementation has shown the contrast between individual level efficacy and population level effectiveness can be quite dramatic’ [8].
With the millions of people currently on treatment expected to graduate to more expensive, second and third line treatment to combat the onset of viral resistance, alongside recent data on the benefits of offering ART to HIV-positive people regardless of their CD4 count, the future of the global AIDS response looks decidedly more expensive and fiscally uncertain (see Fig. 2). For every person placed on treatment in 2014, for example, about two people became infected with HIV; prompting a recent high level meeting at Harvard to suggests that ‘countries may not be aware of the extent of the “hidden debt” of long term commitments [of funding the epidemic] particularly by putting patients on ART….’ and concluding that ‘it is important for countries to have immediate conversations with Ministries of Finance and other stakeholders about the true costs of the potential long-term commitments’ [2].
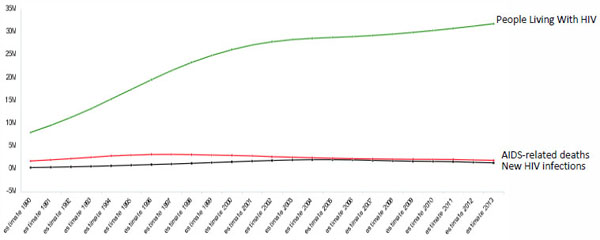
Yearly number of people living with HIV, new HIV infections, and AIDS related deaths, 1990-2013 [3].
Although the prices of first line ARVs have declined considerably over the past decade, the volume of people living with HIV/AIDS has remained unsustainably high [9]. Second line treatment to combat the onset of viral resistance remains beyond the means of developing countries; a position set to become more pressing as increasing numbers of people across the developing world develop resistance to first line treatment. Moreover, with the pool of people living with HIV set to be replenished with new entrants through infections, the implied structures and programmes to cover even the lowest estimate of projected treatment needs in the coming years are beyond the means of governments across the developing world particularly in Africa. Future costs remain difficult to gauge with accuracy because of the number of variables, incomplete/ineffective monitoring of patients and inadequate laboratory facilities; and the unavailability of routine viral load monitoring in poor countries poses serious challenges for the clinical determination to induct patients onto second line treatments [10].
Moreover, although various modelling exercises have been conducted, the likely costs of second and third-line treatments are unclear, although one limited study in the US showed that ‘…second and third-line treatments were both significantly more expensive than first-line treatment, increasing costs by 24% and 41% respectively’ [11]. Furthermore, as HIV and AIDS treatments are set to extend in scope and lengthen in time, critical infrastructural and professional deficiencies are already apparent: The management of HIV increasingly requires a multidisciplinary testing approach involving haematology, chemistry, and tests associated with the management of non-communicable diseases; thus, added expertise is needed. This is further complicated by additional human resource requirements and the need for continuous training, a sustainable supply chain, and reimbursement strategies. It is clear that, to ensure appropriate national implementation either in a tiered laboratory model or a total decentralized model, clear, country specific assessments need to be conducted [12].
AIDS Response in the Era of Sustainable Development Goals
Using World Bank data from 2012 to update estimates of HIV/AIDS resource needs and projecting forward to 2020, Fig. (3) gives some indication of the growing gap. In total, the required financing for all developing countries is likely to increase substantially in the coming years. For example, in 2014 about 60% of Africans living with HIV were receiving treatment under World Health Organisation (WHO) 2010 eligibility guidelines (CD4 350) and long-term projections indicate that the number of people living with HIV/AIDS in Africa by 2050 could reach 80 million [13].
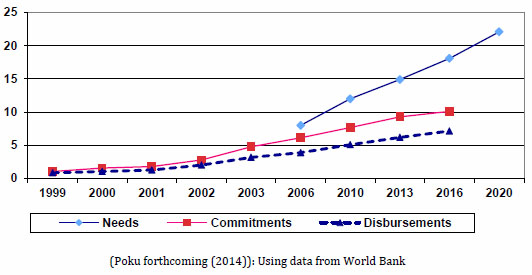
Estimated financial needs, commitments and disbursements (US$ billion).
Overseas Development Assistance (ODA) provides the most compelling image of the nature of the current uncertainties. After a noticeable decline during the 1990s, total ODA financing increased substantially from US$53.6 billion in 2000 to US$87.1 billion in 2008 (in constant 2002 US$) [13]. The increase was entirely driven by new global commitments to fight HIV, TB and Malaria [14]. As a result of the sub-prime market collapse of 2008 global commitment to ODA declined by 13% during 2009-2010 though there was a modest rebound of 8% in 2012 over 2011 [15]. The $28-50 billion estimated by UNAIDS for meeting universal access during the period 2010-2015 (Global Fund 2010) and the $15 billion requested by the Global Fund for HIV/AIDS, TB and Malaria (Global Fund) over 2014-2016 is unlikely to be available [16].
This decline in new financial commitments for HIV is only one of a myriad of changes we are seeing across the donor landscape; with retrenchment of bilateral donor support for HIV activities in place of basket support through Global Fund and an in country shift towards a focus on Sexual and Reproductive Health and Rights (SRHR) along with Maternal health [4]. A key to understanding this shift lies in the emerging post Millennium Development Goals (MDG) framework; the so called ‘Sustainable Development Goals’ or SDGs for short. The principles around the SDGs were presented to the September 2013 United Nations (UN) General Assembly Special Event Towards Achieving the MDGs [17]. At this event, Global Leaders agreed on the need to pursue a coherent, balanced approach to the three dimensions of sustainable development (social, economic and environmental) in a single framework with one set of goals. The Outcome Document also emphasized the need to build on the MDGs, to complete unfinished business, and for future goals to be ‘universal in nature and applicable to all countries, while taking account of differing national circumstances and respecting national policies and priorities’.
Sustainable development goals [19].
|
Cluster1 Poverty eradication Promoting equality Cluster2 Gender equality and women’s empowerment Education Employment and decent work for all Health and population dynamics Cluster3 Water and sanitation Sustainable agriculture, food security and nutrition |
Cluster4 Energy Economic growth Industrialisation Infrastructure Cluster5 Sustainable cities and human settlements Promote sustainable consumption and production Climate |
Cluster6 Conservation and sustainable use of marine resources, oceans and seas Ecosystems and biodiversity Cluster7 Means of implementation Cluster8 Peaceful and non-violent societies, capable institutions |
The Member States’ Open Working Group on Sustainable Development Goals (OWG) has since released its 19 focus areas and organised them in eight clusters, from which it aims to build consensus on identifying Sustainable Development Goals (SDGs) and accompanying targets [18]. Looking at the proposed SDGs in (Table 1), two observations stand out: first, unlike its predecessor (the MDGs), the SDGs appear to not recognise HIV and AIDS as a distinct cluster or focus area; second, the majority of the 19 focus areas reflect the fact that epidemiological and demographic transitions have imposed a complex burden of infectious diseases alongside non-communicable diseases, mental health, injuries and the consequences of violence, which now dominate global health. As a result, there is increasing awareness that, in many countries, the net effect of the increasing costs of technology, ageing populations and rising public expectations will threaten the financial sustainability of health systems even in high and middle income countries.
As states and stakeholders work to agree on the Sustainable Development Goals (SDGs) that will drive the post-2015 development agenda, it is clear that the global fight against HIV and AIDS will have to compete with the full panoply of Human Development aspirations, including action on climate change, marine conservation, urbanization initiatives and sustainable economic growth. However well-integrated the post-2015 Sustainable Development plan is in prospect, the programmatic difficulties entailed in 17 goals and 169 targets [20] spread across nearly every important aspect of planetary sustainability and human equity are likely to create hard choices.
For the HIV and AIDS response there are a number of discernible risks from the ensuing changes in global health:
- First, the expansion of the post-MDG agenda will inevitably mean that financing for HIV and AIDS programming and support activities will decline. Early signs of this are already evident from the fact that no new specific commitment for the epidemic has been made since 2008. Moreover, global financing for HIV and AIDS declined by 18% during 2009-2013 [15].
- Second, the expansion of the global health priority areas to encompass disease of affluence (such as aging, obesity, diabetes, among others) will move prioritisation for development from a geographical space (North/South or developed/underdeveloped) to thematic issues, which are global.
- Third, as the thematic priorities expand, there will be enormous pressure to collapse the generally vertical HIV and AIDS programmes into the broader health sector of affected countries. The argument will be that doing so will not only ensure the long term sustainability of the HIV and AIDS response, but will also enable the much needed strengthening of health systems to be initiated.
The combined effect of the trends above is that the exceptionalism afforded to the global HIV and AIDS response over the last decade and a half may be coming to an end. Taken together, these developments require the global HIV community to consider how they might best consolidate gains in the battle against HIV; and, indeed, how to ensure that they do not lose ground. Ambitious targets necessitate clear thinking about how to align ends to means, and in view of the decline in funding, the changed and changing donor landscape, the inescapably large and rising costs of retaining millions of people on anti retrovirals and a continuing rise in infections, a long over due rethink about what works in HIV prevention is needed.
Viewed in this light, the ‘Fast Track’ agenda from UNAIDS to facilitate the ending of AIDS as a public health concern by 2030 is ambitious, but timely [9]. As the‘15 by 15’(15 million people on ARVs by 2015) targets were declared to have been met in July 2015, there is no denying the fact that target setting is a powerful motivator for the global campaign to eradicate HIV and AIDS. This realisation has emboldened UNAIDS to call for ever higher aspirational targets: ‘90-90-90’ by 2020: 90% of people living with HIV tested, 90% receiving treatment, and 90% with an undetectable viral load; more recently the ‘Three Zeros’ (see Table 2); and now, ‘Fast Track’ - a strategic drive to end AIDS by 2030. The science behind ‘Fast Track’ draws heavily on what we have learnt of the epidemic over the past three decades; namely, (i) go granular focus on the areas where the HIV epidemic is highly concentrated, and identify the places where services are lacking or not reaching the people in need of prevention, testing, treatment and support services; (ii) sustained commitment by ensuring clearer accountability for front loading investments, achieving financial sustainability and mobilizing resources from both traditional and emerging development partners as well as domestic sources; and (iii) be inclusive and ethical by addressing and protecting the needs and rights of those most affected and marginalized key populations.
Goal: Ending the AIDS epidemic.
| Towards zero new HIV infections | Achieve an 80-90% reduction in new adult infections and among key populations (to 200,000 - 400,000 per year) |
| Towards zero discrimination | Stigma and discrimination faced by people living with HIV (PLHIV) and key populations reduced by 75% from 2010 levels by 2030 |
| Towards zero AIDS related deaths | Achieve universal ART coverage - 80% coverage for all people living with HIV, including key populations, by 2020 and 85% by 2030 and viral load suppression of 95% among people on treatment, resulting in an 80% reduction in AIDS related deaths (to 380,000 per year). |
Behind the seductive language of ‘Fast Track’, with emphasis on prioritisation, geographic emphasis and frontloading resources to areas of greatest need, lies sexually transmitted diseases (STD) epidemiology control ideology. Predicated on computer models, the ideology postulates that even a small number of highly sexually active individuals can maintain an STD epidemic in an otherwise low risk population [21]. The approach is centred on the assumption that this analysis provides a basis for programme efficacy, justifying the targeting of resources to groups assumed to be most critical for transmissions, ‘key populations’ or what used to be known as the 'core transmitters'. As such the imperative message of ‘Fast Track’ is ‘trace them, treat them and educate them to prevent reinfection’. The approach is an excellent example of how international organisations shape domestic programmatic interventions. The pressing question is whether the model fits the reality of what is needed at the programmatic level within countries?
The Ideological Mistakes in Prevention Strategies
In The Wisdom of Whores, a pioneering book published in 2008, author Elizabeth Pisani suggests that the HIV disaster is, at least in part, the result of an ideological obsession among the agencies in the 1990s that ‘HIV is a development problem’; in other words, that the issues to be addressed were poverty, education and women's rights, rather than the more simple base cause - sex. While Pisani is wrong about HIV not being a development problem, she is correct to draw attention to the power of ideological obsession that has distorted the institutional response to the epidemic.
|
Box 1. ABC: Does it Go Far Enough?
The Final Report of the United Nations Commission on HIV/AIDS and Governance (2008) states that the ‘ABC’ approach makes no distinction between the different needs of men and women, and fails to offer African girls real options that are attuned to the reality of their daily lives. Abstinence is unrealistic in an environment in which boys are encouraged to be sexually aggressive and girls are kept in ignorance about their own sexuality. Moreover, calls for abstinence are, of course, meaningless when sexual activity is coerced, or when women and girls feel they must resort to sex as a matter of survival. Being faithful only works if both partners play by the same rules. Yet prevailing norms encourage men to have multiple partners. As one male adolescent in Namibia put it, ‘You can get famous if you have a lot of girls’. Fidelity will do nothing to protect a girl or woman against HIV/AIDS if her partner is unfaithful; nor will fidelity to an older male who is more likely to be infected. Condom use is almost invariably a male decision, and many men remain deeply reluctant to use them. Alternative forms of contraception, meanwhile, which might give greater power to women and girls, are hard to come by. Microbicides are still a distant though foreseeable promise, while female condoms are neither widely available nor easily affordable. Furthermore, although women control them, their use often calls for the kind of negotiation with a partner and the kind of familiarity with one’s body with which few. |
What were these obsessions? The first and simplest to engage with is the obsessive promotion of the ‘ABC’ prevention approach - Abstain from sex, or Be faithful, or use Condoms; the second is the transfer of prevention strategies and ideas focused on condom promotion derived from the gay epidemic in the United States (US) to a very different set of environments in the developing world, particularly Africa; the third is the way the epidemic has been used as a vehicle for mobilising resources for other significant concerns, notably civil society activism. On close examination, much of the civil society activism turns out to have little to do with HIV/AIDS - at least, not in the straightforward way that many in the advocacy industry would claim.
Over the past three decades, many of the institutions charged with the governance of HIV prevention programmes have prioritised ABC as the only way forward, particularly in the developing world. Abstinence, fidelity, or condom use are the successful outcomes of any behaviour change strategy for HIV/AIDS. We have known this since HIV was identified as a sexually transmitted infection, and these are proven goals for all prevention of sexually transmitted infections (STIs). However, what is less well understood is how to bring about A, B, and C. The related programmatic interventions have focused on mass education, with related mass condom distribution, in the process creating the impression that nations are responding and, as such, any demonstrable impacts on new infections must be due to risky behaviour or inflexible cultural norms. The reality, however, is a little more complex and suggest a fundamental misalignment of prevention approaches to the needs of not only countries, but communities of populations within countries. Improved HIV surveillance shows that concentrated epidemics are more widespread than generally believed. Yet, the focus in programmatic interventions remains at the level of the general population, with limited or no knowledge in most countries about the key populations driving the epidemic.
In Ghana, for example, the general population accounts for 15% of infections, while sex workers account for 85% Fig. (4), yet the broad strategy in Ghana, as elsewhere, continues to emphasise a generalized multisectoral response. This reflects a disconnect between the epidemic and the response, one reason for which is the reliance on behavioural survey data, which may indicate a lack of protected sexual contact, without adequate episurveillance data, which would indicate that this may not matter for the general population. This implies that countries urgently need good surveillance data and better monitoring of interactions among groups (such as sex workers and clients, injecting drug users and their partners). The lack of adequate data gathering and monitoring means the epidemic is taking off in several countries. In contrast, in Zambia the general population accounts for 92% of infections, sex workers 6%, and soldiers 2% (Fig. 5). This, along with similar scenarios in other countries in the region, suggests that primary prevention (focused on the uninfected) matters for southern Africa and probably eastern Africa, but secondary prevention (focused on the infected groups in concentrated epidemics) is needed elsewhere.
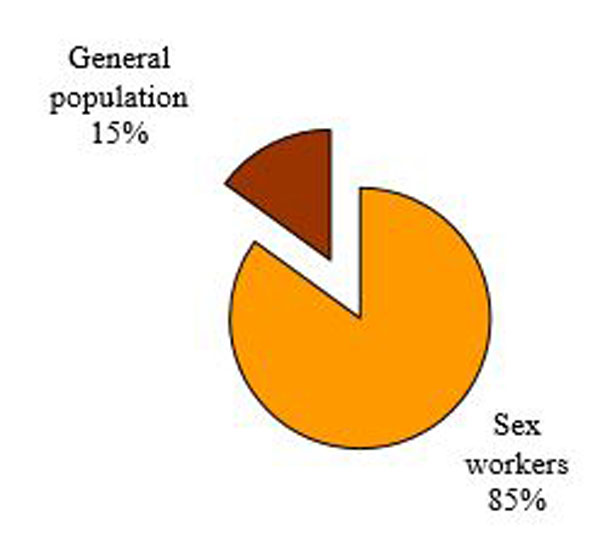
Most HIV infections in Ghana are among sex workers.
Based on this argument, two parallel and interconnected approaches will improve the efficacy of prevention programmes. The first is to better target prevention interventions to specific groups in ways that take into account their risk factors. The second is to expand prevention services to reach groups in underserved areas. The problem with the ABC approach is that the neat alphabetic label confuses the outcomes of successful HIV programmes with the message needed to achieve effective results. It also ignores the strong possibility that each of these components may be more or less effective or relevant depending on cultural, political and economic circumstances, and the stage of the epidemic - early or late.
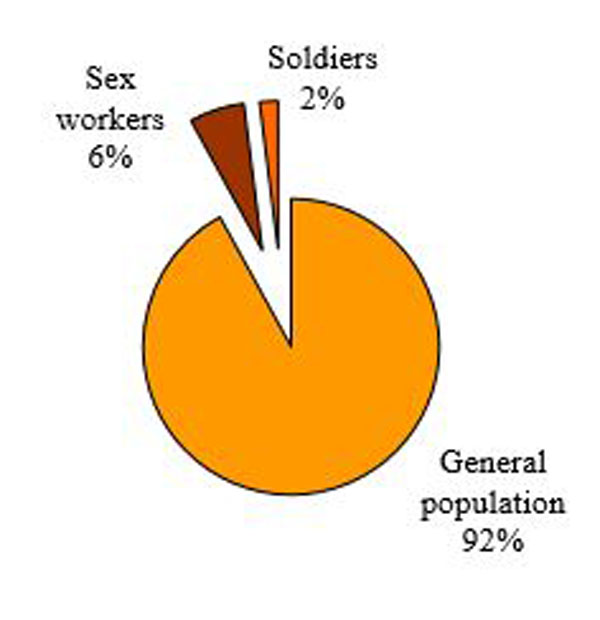
Source of infection in Zambia.
The experience of Uganda is instructive. In its earliest responses, the government encouraged people to talk about HIV and AIDS and the result was a diversity of responses. Getting people to change their sex lives requires addressing their realities. The best way to do this is to encourage those who fund and design prevention programmes to understand these diverse situations and to customise messages to specific local needs; ‘local’ here meaning both geographically and socially local. Pushing for one overarching ‘best’ message will never be effective [22, 23]. Uganda was remarkable in the extent to which it achieved diversity in prevention messages, but this was done by establishing a political environment that encouraged many actors with many messages [24, 25]. Recent regressions are arguably attributable to the focus on treatment at the expense of the traditional method of multi sectoral prevention.
The second ideological obsession is the focus on condom use as an indication of efficacy of prevention interventions. It is obvious that a barrier method prevents transfer of the virus. Condoms have been very important in reducing transmission in heterosexual and homosexual epidemics in the rich countries. In other countries, only Thailand’s success, until recently, in reducing the spread of HIV can be clearly attributed to widespread condom use. Yet it was not to do with condoms alone. The relative success of this strategy had much to do with the Thai government’s strong support for large-scale condom distribution and the institutionalised nature of the sex trade in that country. Even so, as Thailand’s own AIDS Response Program Report states, ‘Access to prevention services has improved and safer behaviours are practiced more consistently; however, the change is not high enough to significantly reduce new infection as targeted. Besides, incidence of [sexually transmitted infections] shows signs of increasing, particularly in young people’ [26].
The emphasis on condoms arose from apparent ‘common sense’ combined with the already installed capacity that existed in the family planning business at the beginning of the epidemic. The first identified outbreaks of HIV were among gay men in the US and Western Europe in the early 1980s. In this highly motivated group, where sex was largely recreational, condoms were a key component of an effective response. Men who have sex with men were familiar with the technology, they had few moral or ideological scruples about using condoms, and if they wished to continue with the bath house culture of the 1970s, then condoms were a necessity.
In contrast, the explosive nature of the African epidemics shows that despite the resources devoted to condom distribution over the past two decades, there has never been sufficient availability of condoms, and where available, people have been very reluctant to use them. Until recently, religious opposition has also been a significant adverse factor. According to UNAIDS, ‘In 2012, the donor community supplied 3 billion male and 32 million female condoms. In sub-Saharan Africa, this translates into eight condoms per man per year and one condom per every 10 women per year. Condom stock outs remain a critical challenge to HIV prevention [and] innovative ways to alert and overcome stock outs are urgently needed’ [27]. While some of the largest countries Brazil, China and India are self sufficient in providing condoms, for many poor countries, the gap between condom needs and donor support means paying for imported condoms with funds diverted from purchases of much needed food, medicine and other necessities.
Though condom promotion looked like a sensible response, it has been singularly ineffective; a point recently made by President Yoweri Museveni of Uganda: ‘in the 90s when HIV infection rates reduced from 18-6% our message was not to resort to condoms but abstinence. We managed to bring down the rates of infection through prevention messages until other people brought in condom use and circumcision. People became complacent… for a young person to get AIDS is to betray their parents who have invested so much in them. If you don’t trust someone, why do you sleep with them just because you have a condom?’ [28].
So, why have condoms been the preferred strategy? The answer is the installed capacity of the birth control business; the fact that the condom strategy worked with gay men in Europe and the USA; and finally the prioritisation of resources for vaccine research, because that was Big Science and, if successful, a good technological fix for a big problem, despite the fact that ‘effective vaccines remain years away’ [29].
Social Nature of Infection
Prevention, and especially the behaviour changes needed to ensure prevention, occur in social and economic contexts, yet they depend on individual decisions. Behaviour change requires far more than having basic knowledge about AIDS, or even being disturbed or concerned about it. Knowledge surveys have demonstrated that more than 95% of the adult population of Swaziland has learned about AIDS and more than 80% know two or more modes of prevention; still the epidemic in Swaziland is out of control, with nearly one in every four adults now infected with HIV and the number of new infections continuing to rise.
Getting people to change their sex lives requires addressing their social (and often economic) realities. It is in this sense that the author Pisani is wrong to suggest HIV prevention is not essentially a development issue: it most certainly is, and it begins with the simple question: why do people get infected with HIV? There are obvious and less obvious answers to this question, with the obvious answer being that a virus passes between one person and another, most often during sex, but also via inadequately cleaned medical instruments, injection syringes, blood transfusion, or from an infected mother to her child during birth. The less obvious answer and it is one that takes us directly onto development is that wider social, economic and cultural conditions affect the likelihood of somebody becoming infected.
In essence we need to examine two major factors: the means to change behaviour, and the propensity to do so. The means to change depends on the physical means, the social status to do be able so, some control over relationships and actions, and certain choices. In the presence of choices and physical means, the motivation or propensity to change becomes a factor. Propensity is dependent on sufficient motivation to never engage in risky behaviour, motivations to shift from a mode of risky behaviour to less risky behaviour, and sufficient motivation to maintain less risky behaviour once in that state. This propensity to engage in less risky behaviour is dependent upon social norms, perceptions of what such behaviour implies about the individual and others, and the perceived reward that this will bring. Taking cognizance of the context or environment in which individual behaviour changes occur will help to precipitate and maintain the changes.
We know that social and economic inequality, including gender inequality, can and does lead to men exercising sexual power over women.What happens in the market, what happens in the public arena, the public examples set by rich and powerful men, terms of trade between producers and purchasers of commodities all of these may affect sexual choices and situations. The fact that women fish sellers may have to facilitate their purchases from fishermen and their sales to dealers by providing sex as well as cash or fish, may seem surprising but it happens, and it happens because men expect it and women feel they have no choice. At another level, wage rate systems that habitually pay women less than men, property laws that give men precedence over women in ownership and inheritance, laws against rape that are not treated seriously by the courts all of these are ways in which broad social conditions provide a breeding ground for HIV.
The social scorn and even violence that afflict sex workers, men who have sex with men, and injecting drug users in many settings, now often exacerbated by HIV stigma, can be an almost insuperable barrier to reaching these vulnerable populations with prevention services, even when resources are available. Many governments refuse to acknowledge the existence of these populations or their right to prevention services, setting inappropriate prevention priorities that endanger those at risk and squander the opportunity to bring the epidemic under control at an early stage. Moreover, many governments continue to pursue failed punitive policies toward sex work and drug use, driving those at risk of HIV infection further underground and enhancing the spread of the virus through incarceration or forced (and ineffective) drug treatment. Although effective prevention interventions for sex workers, injecting drug users, and men who have sex with men are well known, scaling them up will depend fundamentally on protecting the rights of these vulnerable populations, reversing harmful government policies, and setting appropriate priorities.
So where do we go to from here with prevention? Conventional wisdom argues that the problem is one of scale of bringing a set of proven interventions to those who need them, of moving from projects to national programmes and that the primary obstacle is lack of resources. Indeed, most people in the developing world still do not have access to basic prevention services, and rapid scale up of coverage remains a central priority. There is no doubt, moreover, that the gap between what comprehensive coverage would cost and the resources currently available to developing countries remains large. For some prevention services, notably prevention of mother to child transmission and treatment of sexually transmitted infections, the challenge is indeed primarily that of scaling up, and of strengthening health systems to make this possible.
However, for other critical aspects of prevention, other challenges are at least as important. In the high prevalence, generalised epidemics of eastern and southern Africa, successful prevention will require broad based changes in behaviour. At an individual level, we know that using condoms consistently and having fewer sexual partners can prevent most new infections, but, at a population level, patterns of sexual behaviour have often proved resistant to change. Part of the answer is greater coverage of standard prevention services and provision of basic information and motivation for change through the media, schools, and other channels. This will require more resources, but the experience of 30 years has taught that success will require greater attention to two additional factors, outlined below.
First is that we now understand that the capacity of individuals to change their behaviour and to protect themselves is often very constrained by economic circumstances, by gender inequities, often reinforced by both cultural forms and economic circumstances. Thus, greater efforts should be focused on addressing these broader obstacles to behaviour change, especially the rigid gender roles and inequalities that put both women and men at greater risk. Currently, we are seeing differential vulnerability to HIV - with young women showing the highest incidence. Women’s reduced autonomy in sexual decision making and violence against women both intersect with women’s poor economic situation which further exacerbates their difficulties in negotiating sexual relations. That society condones such violence and that women’s subordinate position is normative attest to women’s status as second class citizens in society. Imagine for a moment society’s response to the full citizen, that is, to men, it is hard to envision social acceptance of generalised rape of men; of men having to carry a pregnancy to term which resulted from coerced sex; of men being thrown out of the homes they have created and the relationships they have nurtured simply because they get sick; yet these are the conditions of women. As a result, we are seeing differential impacts of HIV, with women more likely to be stigmatised and left without care; more likely to face financial difficulties in accessing treatment or care; more likely to be engaged in a form of income generation which offers no legal protection and no medical aid.
Second, one of the greatest lessons of the few relatively large scale HIV prevention success stories is that the impetus for lasting change, and much of the difficult work of addressing deeply rooted cultural norms, must come from communities themselves. Community involvement is essential in reaching key marginalised and vulnerable populations at greatest risk of infection and at risk of infecting others. Donors and national governments can do much to stimulate, support, and expand this local response, but must do so in ways that respect and enhance the leading role of communities and local civil society. An approach which is centred around community mobilization does not pre empt the possibility of setting priorities; rather it does so with the assistance of communities. The foci of assistance need to be complemented by a more general mobilization and sustained by appropriate forms of assistance, by the availability, accessibility and affordability of the required goods and services and by appropriate legal, ethical and human rights policies and practices.
CONCLUSION
The progress made against HIV and AIDS in the last fifteen years has rightly been hailed as an unprecedented, extended expression of global solidarity; as a first order organizational and political achievement; and as a unique programme combining biomedical and behavioural interventions; sustained, in country innovations in prevention; an astonishing marshalling of financial resources; and feats of consensus building and coordination against all manner of national, organizational and cultural divides. With 15 million human beings now on life saving antiretrovirals it is perhaps difficult to appreciate the intimidating odds against meeting that target at the outset.
However, what remains to be done is no less daunting than what we faced at the Millennium [30]. The momentum achieved during the course of the MDGs is of invaluable political and normative importance, but it is likely to be an unhelpful guide to the next fifteen years in respect of either the disease dynamics or the world of fiscal and political possibilities. In any event, the normative force of sustained effort and the early achievement of the ART enrolment target will diminish rapidly; and all the more swiftly if the world ceases to perceive HIV and AIDS as a continuing global health emergency. As such, UNAID’s ‘Fast Track’ strategy is timely.
The encompassing, strategic challenge for the next fifteen years is this: because of profound shifts in the donor landscape, we are obliged to conceive and enact a transition in how the fight against AIDS will be funded and organized, even as we work to secure and consolidate the gains we have made and undertake to more than double the number of people on ART.The strengthening and enlargement of programmatic activities at the heart of the 2030 campaign must be newly enabled, on the basis of reconfigured donor recipient and other key relationships. The challenges this will generate will reach all levels and nearly every particular of the global AIDS response.
Revitalising prevention initiatives is an urgent priority. Without renewed, effective prevention programmes, we run the risk of losing ground to HIV, even as we prepare to extend treatment coverage to millions more people. Linked to the full panoply of tailored interventions and education, there are several other issues related to the quality of the current ART regime: inadequate screening of patients and follow-up monitoring of drug regime adherence, dealing with escalating drug resistance, patchy viral load testing services, and breaks in the drugs supply chain. The triumph over the past decade or so is more a reprieve than a victory one that requires consolidation through renewed effort. The key to not losing ground is in the prevention of new infections.
Success in prevention is tied up in complex ways with people’s diverse life situations, with property, kinship alliance, ritual and religious beliefs, ancestors and gender relations, income and inequality, land and livelihoods [31]. The fact that prevention initiatives have been only marginally effective demonstrates that ‘one size does not fit all’; there is no single model that works, nor works everywhere. The balance between prevention, treatment and impact mitigation will be specific to each country. The specific local cultural, political and material circumstances will influence the content of any particular programme. Furthermore, countries will need to break down the epidemics into their geographic, social and economic components, in order to frame and target national prevention programmes in ways that increase their efficacy. This must take place in an environment that promotes the possibility of open and honest discussion of sexuality and dying by confronting some uncomfortable cultural and societal truths.
For three decades it has been the position of many observers of this grotesquely pervasive epidemic that politics, not medicine, has been its dominant feature. Consequently, it is in the political arena in which a solution has to be conceived and enacted to enable a revolution in HIV prevention, as much as in medical terms. The challenge for all governments is to understand just how little we have in the armoury, how cunning is the enemy, and how important it is to seek solutions in the diversity of responses which have been shown to be possible, from within the richness of their particular circumstances. Uniform prescriptions from outside may end up wasting resources and lives [32, 33].
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


