RESEARCH ARTICLE
Factors Supporting and Inhibiting Adherence to HIV Medication Regimen in Women: A Qualitative Analysis of Patient Interviews
Oluwakemi Fagbami*, 1, Adetokunbo Oluwasanjo1, Carrie Fitzpatrick2, Rebecca Fairchild1, Ann Shin1, Anthony Donato1
Article Information
Identifiers and Pagination:
Year: 2015Volume: 9
First Page: 45
Last Page: 50
Publisher ID: TOAIDJ-9-45
DOI: 10.2174/1874613601509010045
Article History:
Received Date: 19/1/2015Revision Received Date: 30/3/2015
Acceptance Date: 2/4/2015
Electronic publication date: 15 /5/2015
Collection year: 2015

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Adherence to antiretroviral therapy reduces morbidity and mortality; however rates of non-adherence are variable among women for unclear reasons. This study was a single-center qualitative analysis of interviews with 18 female HIV-positive non-adherent patients (defined by virologic failure) to explore psychosocial factors impacting adherence. Factors identified were categorized as promoting, inhibiting or having no effect on adherence. Three themes, characterized as social factors, illness factors and other societal pressures, were identified. Medical systems support, family support and compliance for children were most commonly identified as promoting adherence, while psychiatric comorbidities, lack of medical systems support and side effects were identified most often as inhibitors of adherence. While stigma was frequently identified, it was not seen as a barrier to adherence. Enhancing relationships between patients and their providers as well as their community support systems are critical avenues to pursue in improving compliance. Interventions to promote compliance are important avenues of future research.
INTRODUCTION
Adherence to Antiretroviral therapy (ART) reduces morbidity and mortality, risk of viral resistance and transmission to sexual partners and children. However, for ART to be effective, adherence must be nearly complete, as even above average levels of adherence (80-90%) are associated with treatment failure in 50% of patients [1]. Non-adherent patients are noted to have an overall mortality risk that is 3.8 times higher than that of adherent patients [2]. Adherence is therefore of critical importance to individual patient outcomes as well as an overall public health concern [3].
Only 88% of women living with HIV in the United States are diagnosed, with 45% noting regular access to healthcare. Of these, 32% have their disease well controlled on ART [4]. Reported rates of non-adherence to ART in women range from 33-75%, a rate which is generally worse than reported non-adherence rates in men [5-7]. Women have also been found to have increased viral rebound following non-adherence episodes [8], making their non-adherence behaviors potentially more morbid. Factors that have been associated with non-adherence in women include depression [1, 8-10], alcohol or substance abuse [1, 10, 11], medication side effects [10, 12, 13], stigma [11, 13, 14], lack of social support [1, 8], and poor patient-provider relationships [1, 9, 12, 13, 15]. While no demographic traits can reliably predict adherence [14], patient attitudes and beliefs have been identified as important predictors of adherence [16].
Despite the advent of simpler ART regimens with better side effect profiles, non-adherence still remains an important public health concern [1, 13, 14]. We hypothesized that women with less than optimal compliance with ART would have important and potentially causal attitudes, beliefs and unmet psychosocial needs that contributed to their non-adherence. This study was a single-center qualitative analysis of interviews with female HIV-positive non-adherent patients. It was aimed at exploring both positive and negative factors impacting adherence.
METHODS
This study was a qualitative analysis of individual patient interviews. Using purposeful sampling [17], participants were recruited from the Reading Health’s Center for Public Health. Individuals were chosen for recruitment from the 185 female patients aged older than 18 who carried the diagnosis of HIV infection. In order to identify a subset who may have been non-adherent to medication regimens, we selected the 105 records of those with any evidence of failure of virologic suppression, defined by a viral load of >200 copies/ml in patients already prescribed antiviral medications (as has been used by the HIV/AIDS bureau as a benchmark of treatment failure [18].
Forty patients without either viable listed contact information or could not be reached on successive calls were further excluded, leaving 65 patients who were contacted about our study and asked to participate in a one hour interview. Forty agreed to participate in the study and were scheduled for formal consent and interview, and eighteen patients completed the interview process. Participants were compensated with a $25 gift card as compensation for their time.
A semi-structured interview guide [17] was developed from an extensive review of the literature to broach potential barriers to adherence to therapy in women. A priori topic areas [19] identified included economic issues (job security, financial responsibilities, medication costs and co-pays), family issues (including need to care for children and the impact of support from loved ones), psychiatric issues, substance abuse issues, educational factors (including formal education and understanding of disease), healthcare logistics (appointment timing, availability of transportation), trust in providers and healthcare systems, overall health issues and their impact on adherence, medication side effects, pill burden issues, use of non-traditional medicines, spirituality issues, and the patient’s own sense of responsibility for their health.
Two female interviewers (including one physician (either OF, AO) or one certified nurse practitioner (RF), along with a communication specialist with extensive experience with qualitative research (CF) performed all of the interviews. One interview was with a Spanish-speaking only participant and was performed with the aid of a certified female Spanish interpreter, while the rest were performed in English. All interviews were de-identified and recorded on audiotape and transcribed by the hospital’s transcription service.
An initial inductive thematic analysis [20] of the data was conducted independently by the four principal investigators (OF, AO, AD, CF). Based on this initial review, a detailed codebook was developed from the previously identified themes and those detected from the initial thematic analysis. All four investigators then re-reviewed the text and coded the narrative. Finally, the four investigators reconvened to reach agreement on the identified themes, and determined whether the identified theme was helpful to compliance, a barrier to compliance, or had no effect, with each decided by consensus. The unit of analysis was a phrase, sentence or paragraph of any particular section of narrative that was a potential explanatory factor in non-adherence. Quotes were corrected for grammar and changed (indicated by brackets) to improve readability and to make the author anonymous.
This study was approved by the Reading Hospital Institutional Review Board (IRB 009-12)
RESULTS
Eighteen females completed interviews. The average age of participants was 47.7 (SD: 10.2) years. Ten participants (56%) were Caucasian, five (28%) were Hispanic and three (17%) were African-American. Six (33%) were currently employed at time of the interview. Sixteen (89%) had children, including eight (44%) who currently were caring for those children. Twelve subjects (67%) had completed at least a high school education, including five (28%) that had schooling beyond high school. Eleven (61%) noted a past history of substance abuse.
Researchers examined the transcript and three emergent themes (social factors, illness factors, and other societal pressures) were derived after data saturation. The most commonly represented theme had to do with social factors, described 175 times by subjects (Table 1, Figs. 1, 2). We identified seven subthemes to social factors, including medical systems support (n=69), stigma (n=26), family support (n=29), compliance for children (n=21), community support (n=13), faith (n=10), general life experiences (n=7).
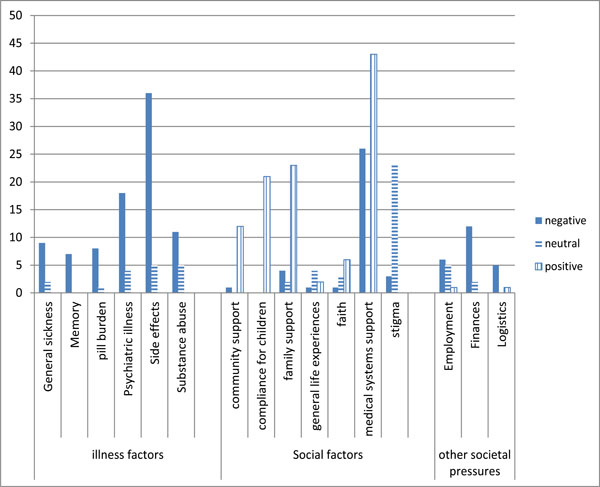 |
Fig. (1). Bar chart of themes and subthemes showing impact on adherence. |
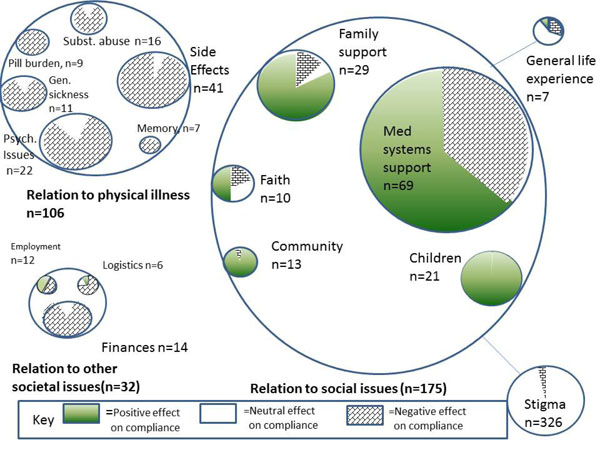 |
Fig. (2). Schematic diagram of themes and subthemes. |
Total theme and subtheme counts.
| Theme | Subtheme | Negative | Neutral | Positive | Total n |
|---|---|---|---|---|---|
| Illness factors | General sickness | 9 | 2 | 0 | 11 |
| Memory | 7 | 0 | 0 | 7 | |
| pill burden | 8 | 1 | 0 | 9 | |
| Psychiatric illness | 18 | 4 | 0 | 22 | |
| Side effects | 36 | 5 | 0 | 41 | |
| Substance abuse | 11 | 5 | 0 | 16 | |
| Illness factors (n) | 89 | 17 | 0 | 106 | |
| Other societal pressures | Employment | 6 | 5 | 1 | 12 |
| Finances | 12 | 2 | 0 | 14 | |
| Logistics | 5 | 0 | 1 | 6 | |
| Other societal pressures (n) | 23 | 7 | 2 | 32 | |
| Social factors | community support | 1 | 0 | 12 | 13 |
| compliance for children | 0 | 0 | 21 | 21 | |
| family support | 4 | 2 | 23 | 29 | |
| general life experiences | 1 | 4 | 2 | 7 | |
| faith | 1 | 3 | 6 | 10 | |
| medical systems support | 26 | 0 | 43 | 69 | |
| stigma | 3 | 23 | 0 | 26 | |
| Social factors (n) | 36 | 32 | 107 | 175 |
Under the theme of social support, support from the medical system was the most commonly identified subtheme. Perceived support from the medical system (or its noted absence) was a critical factor in adherence and non-adherence. One subject who described her experience with the medical system as very positive told us this:
“If it wasn’t for her <the clinic nurse practitioner> I wouldn’t have complied at all. It’s just really hard, I mean, you know, you’re going to make me cry, it’s hard to find people that you connect with, you know? She was my caretaker, my friend, and my therapist… a little bit of everything that sometimes you just need.”
However, several described the opposite effect on adherence from the healthcare system:
“<25 years ago>They put me on AZT. I took a pill. I had had a really bad nose bleed, and I called the nurse and told her “look, whatever’s in this thing made my nose bleed”. She told me that it didn’t, so I went and found me a pill book and in the book it said AZT could cause nose bleeds, and then I knew she didn’t know what she was talking about and I haven’t taken anything since.”
Almost every participant described a poignant story of the stigma they felt as a result of their disease. Surprisingly, their descriptions were matter-of-fact analyses that did not seem to impact their adherence. One illustrative quote was:
“I’m not scared that <family and friends> would find out, it wouldn’t affect me in any way, I am who I am and if you can’t accept me for who I am, then the heck with you, right? I’m going to live my life the longest I can.”
Personal family support was also identified as a generally positive factor in adherence (23/29, 80% of comments), and played a positive role with regards to living with HIV/AIDS. One subject described it this way:
“…<My daughter>she takes care of me. When I’m down and out that I can’t take care of myself ...she makes sure I’m taking my medications, she’s always there for me.”
Another said, “The devil’s around the corner of the neighborhood every turn you take, so, you gotta have your s--t a little bit together to live down in the hood. If it wasn’t for my family, it would be very difficult because I can live without other people but not like my mom or my sisters.”
Another important subtheme was identified in subjects that cared for children. They nearly uniformly identified that taking the medicine for the sake of their children was a positive factor in their adherence. No one identified children or child care as a barrier to adherence. Two illustrative quotes were:
“… I remember when I was first diagnosed, you know when people get that news, everybody takes it differently. You want to go into a deep depression, you feel hopeless, … I was thinking of my sons’ graduation and how I would like to be there to see them graduate. You know, that gives you the motivation to take care of yourself.”
“… When I was pregnant with him, I was on the AZT and I felt so horrible on that, and that was the medication I had tried before I even got pregnant, and I couldn’t take it, but to help my son, I took it. I stayed on it the whole time.”
The second major theme identified in compliance had to do with illness factors, identified 106 times. The vast majority of comments in this theme (83%) were coded as inhibitors of adherence, with the rest coded as neutral to adherence. Subthemes identified included medication side effects (n=41), psychiatric illness (n=22), general sickness issues (n=11), substance abuse (n=16), pill burden (n=9), and memory issues (n=7). Under illness factors, medication side effects were a significant barrier to adherence in most that noted them (36/41, 88%). A quote that captured this sentiment was:
“I was getting diarrhea and I drive almost an hour to work every day so I just couldn’t take the side effects. I can’t be showing up at work and having a reaction at work, or on the way to work, or if you’re late more than 2 or 3 times in one week then you get written up and so if I had to go on the way to work I couldn’t stop and then.”
Psychiatric illness was also cited as a major barrier to compliance. One subject noted:
“When I’m in my depression and not complying with my meds or my mental health stuff, I just stay by myself. I don’t answer the phone, the door, nothing. “
Substance abuse negatively impacted adherence in most subjects who described this condition (11/16, 69%) with no impact in the others (5/16, 31%) (Figs. 1, 2). One subject told us:
“The only time I get in-in the absent mode is when I’m back in my addiction mode because I was told, ‘do not smoke crack, do Cocaine, and take your med’s because I’ll make myself resistant. So that’s the only time I don’t listen. I gave up my nursing career for my addiction, my marriages, … that was like my best friend, my lover, you know, it was like nothing could make me feel any better than that shot of Coke, it was just like really good.”
Several (n=7) described having specific problems with their short-term memory, and felt this negatively impacted their adherence despite their desire to overcome it (Figs. 1, 2).
One participant described:
“I think that would just make my whole life much easier if I could just not forget what I was doing half the time. That has been my major problem with my medication and my adherence. From cooking to everything, you know, you think about short term memory how much it how it impacts everything from taking medicine from going to appointments – I have forgotten appointments. I’ve developed all kinds of new gadgets because I just keep putting stuff in there and have it putting up timers and it’s very difficult. The number one problem for adherence would be the memory. “
The third major theme identified by the authors as relevant to adherence was characterized as ‘other societal pressures’. Subthemes for this included finances (n=14), logistics (n=6) and employment/job issues (n=12). These factors were nearly all perceived as barriers (23/32, 72%) or neutral to adherence (7/32, 22%).
One illustrative quote that highlights patients’ struggles with adherence related to work and finances was:
“I am supposed to be making payments every month, which I have not made, so I haven’t even made a doctor appointment yet, it is hard for me when it is busy at work because I do not have any sick days, I can’t really ask for a day off because I don’t have any sick days left. If it were slow, then I could say, I really need to get in to see a doctor, and again, they don’t know that I am dealing with HIV.”
DISCUSSION
We found that relationships with providers, children, family, and community were the most common factors with a positive effect on adherence. Similar to our findings, other authors noted positive association between strong patient-provider relationships that included open communication and respect were associated with better adherence [7, 9, 11-13, 15, 21].
Conversely, we found that poor patient-provider relationships were a major impediment to adherence. Other authors report similar results, specifically noting that trust issues and lack of perceived empathy from providers were associated with non-adherence [1, 7, 9, 12, 13, 22].
While one author found negative relationship between adherence and childcare responsibilities [7], our findings mirrored those of Wood et al. [10], in which compliance for the sake of dependent children was noted as a universally positive factor in adherence. Similar to others, we identified psychiatric issues, including alcohol and substance abuse [1, 10] and medication side effects [1, 7, 9, 10, 12] were important barriers to adherence. While stigma from family, providers and the general community was a nearly universal theme represented in our interviews, we did not identify a negative impact on adherence compared to other studies [7, 13, 14, 23].
This study used virologic failure as one of the major inclusion criteria, allowing us to capture the voices of women with an objectively documented treatment failure measure associated with their subjective narratives of non-adherence. Our semi-structured interview method allowed us to identify some patient-centered themes that often do not emerge from studies using structured written surveys. The major limitations of this work include that it was a single center study on a small number of subjects, making it difficult to generalize the results to other communities and socioeconomic groups.
Identification of non-adherence is a critical part of care of the patient with HIV. We echo the recommendations of others who suggest that adherence should be directly measured through readily available methods such as patient surveys, pharmacy refill data [16], as well as objective laboratory tests such as virologic failure for those on ART. Depression screening should be performed at regular intervals, and intervention resources should be provided at the location of the screening, as depression has been found to be a major barrier to adherence in multiple studies as discussed above. When non-adherence is identified, interventions should be patient-based and targeted to match barriers identified in women’s daily lives, including coping with side effects as well as substance and alcohol abuse [7, 14, 22]. As much as possible, continuity of care should be maintained to establish and preserve confidence in the medical system due to the huge impact this factor has been shown to have on adherence. This will likely foster strong patient provider relationships, hence impact adherence positively. One future avenue of research could include the effectiveness of interventions to help providers build rapport with patients. Motivational interviewing techniques, voice and text reminders and use of outreach resources [16], including peer group support [12], all deserve further study of their direct impact on adherence.