All published articles of this journal are available on ScienceDirect.
Socio-Demographic and Behavioral Factors Associated with the Desire to Procreate Among Patients Living with HIV in Gabon
Abstract
The desire to procreate in patients living with HIV (PLHIV) has been seldom investigated in Africa, particularly in Gabon. The aim of this transversal and descriptive study was to analyze the socio-demographic and behavioral factors associated with a desire to have children in a cohort of PLHIV. The study included 442 patients, predominantly females [79.9% (337/422)], and those with a secondary school education [64.2% 271/422)]. The highest prevalence of HIV was found in patients aged 30-39 years old (44.3%), of which 59% (249/422) were unemployed. The desire to have children was noted in 78% (329/422) of patients, of which 82.4% (271/329) were treated with antiretroviral drugs; this was significantly higher in subjects under 40 years versus those over 40 years old [81% (268/329) versus 19% (61/329), p<0.001]. Sero-discordant couples represented 33.4% (110/329) of patients. The frequency of patients with the desire to have a child was significantly higher when patients wanted to hold the status of parent of a child [77% (255/329) versus 23% (74/329), p<0.001]; this was influenced by the partner's desire [60% 197/329 versus 40% (132/329), p< 0.001], as well as by the absence of weight loss [56% (185/329) versus 44% (144/329), p<0.001]. The average number of children was significantly lower in patients with the desire to procreate compared to those with no desire to have children [1.7 versus 3.2, p<0.001]. These first observations in Gabon highlight the importance of the desire to have children in PLHIV and sero-discordant couples, and they show the level of interest in developing assistance methods for procreation and family planning programs to help this population, as well as to reduce the risk of mother-to-child HIV transmission.
INTRODUCTION
Human immunodeficiency virus (HIV) infection remains a major public health issue, particularly in sub-Saharan Africa countries where high levels of HIV transmissibility and morbidity-mortality are observed with an important socioeconomic impact [1]. Since 1981, the majority of the HIV-infected population lives in countries with limited resources in Africa. According to the 2009 report from the World Health Organization (WHO) and the Joint United Nations Program on Acquired Immunodeficiency Syndrome (AIDS) (UNAIDS), 2.6 million individuals are newly infected by HIV every year, 33 million patients live with HIV (PLHIV), and there are 1.8 million cases of AIDSmortality annually worldwide. Consistently, with about 70% of PLHIV and 72% of global AIDS-related deaths, Sub-Saharan Africa is the most affected region worldwide. In the absence of preventive actions and expanded treatment, UNAIDS estimations indicate that approximately 68 million people with AIDS will die between 2002 and 2020 [2] in the 45 countries most affected.
Interestingly, the number of people receiving antiretroviral treatment (ART), which was 3 million in 2007 and increased to 6.7 million in 2010, will reach 11.6 million in 2015. Meanwhile, the number of new infections fell from 2.7 million in 2007 to 1.3 million in 2010, with a projected rate of 1.0 million in resource-limited countries by 2015. This exponential increase in the number of patients receiving multiple antiretroviral therapies has been facilitated by the Universal Access Initiative and the significant increase of funding to African countries by international partners (Global Fund, PEPFAR, World Bank, UNICEF, etc.), nongovernmental organizations, and bilateral and multi-lateral cooperation. These data support the fact that the accessibility to ART has become a reality and that results obtained are satisfactory. Indeed, improvement of the quality of life for patients, the increased life expectancy of the general population, and the reduction of new infections and AIDS deaths by 25% over the last 5-10 years have been observed [3-5]. In this new context, within which the care and accessibility to ART have improved for PLHIV, many affected couples living in Africa practice their sexuality and manifest their desire to procreate or to adopt children [6-8]. However, the decision of whether or not to have children remains complex and influenced by various factors, including the possibility of mother-to-child HIV transmission and/or the likelihood that one or both parents could die prior to the child reaching adulthood [9]. Such difficulties are overcome in developed countries where implemented policies and strategies of medically-assisted procreation (MAP) exist for PLHIV [10-12].
In Gabon, recent observations have shown that there are 63,903 PLHIV, with an increase in HIV infection prevalence from 1.8% to 5.2% between 1986 and 2009 [13-15]. However, data obtained from young women aged 15-24 years attending antenatal clinics showed an increase in HIV prevalence from 3.6% to 4.8% between 2007 and 2009. In the same period, 5,000 new infections and over 2,000 deaths were recorded, particularly in patients aged 30-34 years old [13-15]. Since the beginning of the HIV epidemic, there have been no lines to assist couples of patients wishing to procreate or adopt a child in Gabon or in sub-Saharan African countries, while medical teams have observed an increase in requests for reproduction among PLHIV. The national experts proposed to increase the number of health authorities and medical staff, and to inform patients with the possibility of establishing a national medical aid for procreation (MAP). These structures will be useful for the monitoring and medical care of PLHIV and sero-discordant couples with the desire to procreate, so as to prevent mother-to-child HIV transmission during the peri- and post-natal periods.
Therefore, because little is known about the socio-demographic and behavioral factors associated with the desire to procreate or to adopt a child in Gabonese or sub-Saharan PLHIV couples with ART, we decided to conduct this pilot study on a cohort of 490 patients.
PATIENTS AND METHODS
Legal and Ethical Considerations
The study was conducted according to clinical practice policies and national guidelines for research in the Republic of Gabon. Patients consented freely before being included in the study.
Type and Place of the Study
This is a multicenter, transversal, descriptive study using semi-direct inquiry designed to analyze the desire to procreate among HIV-infected patients. Each patient included in the study was interviewed during a medical consultation. The study was conducted between June 1, 2010 and May 31, 2011 for a period of 12 months in Libreville, the capital of Gabon, a sub-Saharan African country of 1,500,000 inhabitants. The HIV sero-prevalence and cumulative incidence rates of PLHIV in Libreville were 7.2% and 63,903 versus 5.2% and 447,321 in Gabon between 2002-2005 and 2009, respectively [13, 15]. The study took place in three centers of public support for PLHIV in Libreville: the Infectious Diseases Service of the Foundation Jeanne Ebori (FJE), the Libreville Hospital Ambulatory treatment centers (LH-ATC), and NKEMBO Hospital (Nkembo H).
Patient Inclusion Criteria
After screening, the female or male PLHIV who met the following criteria were included in the study: over 18 years of age, provided consent to be included in the study, presented with documented HIV infection, and were either receiving or not receiving ART during medical consultations between 1996 and 2011 in one of the three study sites during the study period. The patients’ data were collected between June 1, 2010 and May 31, 2011.
Exclusion Criteria
PLHIV with undocumented HIV infection, those not recorded in the medical file, and/or those who were unable to provide consistent responses to the consent questionnaire were excluded from the study. All patients that were screened and included could still withdraw from the study with consent from either the patient or a family member.
Expected Number of Patients
n = number of patients desired
where,
z = gap set at 1.96 for ᾱ = 0.05 and confidence interval (CI) = 95%
p = proportion of HIV patients with the desire to procreate
q = range of the event
d = degree of accuracy to 0.05
Assuming p=44% is the proportion of PLHIV who want to have a child according to a study conducted in Abidjan [18], and assuming CI=80%, α=5%, β=20% and 1 - β=80% (power) and a 5% accuracy level, the number of patients to be included was 394. With a lost sight and withdrawal from the study rate of 5%, it was desired that 414 HIV-infected patients be included.
Statistical Analysis
Data were expressed as the mean (range), staffs, and percentages, and they were analyzed by the chi-squared test and Fisher's exact test for the comparison of proportions using Epi-Info 3.5.1 software. Factors associated with the desire to procreate were searched using the prevalence ratio and its 95% confidence interval. A p-value of 0.05 was considered significant.
RESULTS
General and Demographic Characteristics of the Study Population
During the 12 months of data collection, 490 PLHIV were screened in the three sites chosen for the study - namely, the Fondation Jeanne Ebori Hospital (FJE), the Libreville Hospital Ambulatory treatment centers (LH-ATC), and NKEMBO Hospital (Nkembo H). From these centers, 86.1% (422/490) patients were included in the study, 13.9% (68/490) were excluded for several reasons including declining to provide consent (40 cases), an age less than 18 years (15 cases), or unconfirmed serology (13 cases).
The 422 included patients were classified as either category B (as per the HIV/AIDS Atlanta Center for Diseases Control classification; CDC, Atlanta, USA) or as stage 3 from the World Health Organization (WHO, Geneva, Switzerland) classification; of them, 83% (350/422) were treated with antiretroviral drugs.
In all, 87 (20.6%), 264 (62.5%), and 71 (16.8%) patients included in the study were recruited from the Fondation Jeanne Ebori Hospital (FJE), the Libreville Hospital Ambulatory treatment centers (LH-ATC), and NKEMBO Hospital (Nkembo H), respectively. There was an increase in the average proportion of screened patients with a positive HIV test in the three sites between 1996 and 2011: 2.4% [10/422; range: 1.2%-3%)], 24.4% [103/422; range: 8.5%-28.7%], and 73.2% [309/422; range: 69.7%-90.1%] patients between 1996-2000, 2001-2005, and 2006-2011, respect-ively (Fig. 1A).
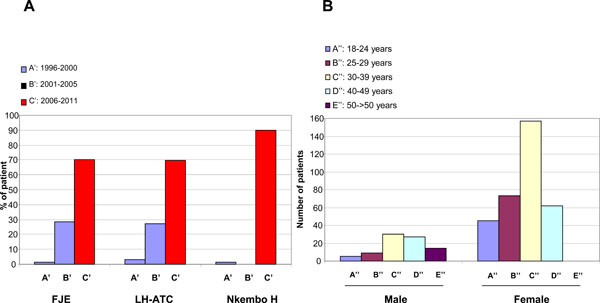
A. Evolution of the proportion of patients who screened positive for HIV at the three hospitals between 1996 and 2011: Fondation Jeanne Ebori Hospital (FJE), Libreville Hospital Ambulatory Treatment Center (LH-ATC), and Nkembo Hospital (Nkembo H). Period A’: 1996-2000, B’: 2001-2005, C’: 2006-2011. B. Distribution of male and female patients according to the following age ranges: A’’: 17-24 years, B’’: 25-29 years, C’’: 30-39 years, D’’: 40-49 years, E’’: >50 years.
The 422 included individuals were predominantly female, representing 79.9% (337/422), and only 20.1% (85/422) males, corresponding to a sex ratio (M/F) equal to 0.25 (data not shown). Their overall mean age was 34±8 years (range: 18-66 years), with the highest HIV prevalence observed in patients aged 30-39 years (44.3%) followed by patients aged 25-29 years (21%), and those 40-49 years (19%) (Fig. 1B). Seventy-five percent [75% (319/422)] of all patients were aged less than 40 years versus 25% (103/422) aged more than 40 years; 52.4% (221/422) of patients lived as part of a couple or were married, and 81.3% (343/422) had parental status (Table 1). From them, a low proportion [10.6% (45/422)] was informed about their children’s HIV test positivity rate (Table 1). The participants were most likely to have a secondary school education [16.4% (69/422) and 64.2% (271/422) were primary and secondary school-educated, respectively], and more than half had no professional activity [59% (249/422)] (Table 1). The majority of patients [71.6% (302/422)] had heterosexual intercourse and condoms were used by 63.5% (268/422) of patients, while few [24.2% (102/422)] knew the HIV-positive status of their partner. Contraception was practiced by one-third of the patients [30.6% (129/422)] (Table 1).
Patients’ distribution with respect to sociodemographic characteristics, sexual behavior, and the desire to procreate. N: number.
| Staff (N=422) | Percentage (%) | |
|---|---|---|
| Marital Status | ||
| Single | 201 | 47.6 |
| Married or coupled | 221 | 52.4 |
| Parent of a Child Status | ||
| Yes | 343 | 81.3 |
| No | 79 | 18.7 |
| Patient with an HIV-Positive Child | ||
| Yes | 45 | 10.6 |
| No | 305 | 72.3 |
| Unknown | 16 | 3.8 |
| Not concerned | 56 | 13.3 |
| School Educational Level | ||
| Primary | 69 | 16.4 |
| Secondary | 271 | 64.2 |
| University | 82 | 19.4 |
| Professional Activity | ||
| Frame-Public function | 104 | 2.8 |
| Storekeepers-Workers | 69 | 5.7 |
| School-Students | 74 | 17.5 |
| Unemployed | 175 | 41.5 |
| Heterosexual Sex | ||
| Yes | 302 | 71.6 |
| No | 120 | 28.4 |
| Condom Use | ||
| Yes | 268 | 63.5 |
| No | 56 | 13.3 |
| Not concerned | 98 | 23.2 |
| Contraception | ||
| Yes | 129 | 30.6 |
| No | 208 | 49.3 |
| Not concerned | 85 | 20.1 |
| Partner’s HIV Status | ||
| Positive | 102 | 24.2 |
| Negative | 136 | 32.2 |
| Unknown | 91 | 21.6 |
| Not concerned | 93 | 22 |
| Fertility Desire | ||
| Yes | 329 | 78 |
| No | 93 | 22 |
| Child's Adoption Possibility | ||
| Yes | 199 | 47.2 |
| No | 199 | 47.2 |
| Not specified | 24 | 5.6 |
| Assumed an HIV-Positive Child | ||
| Yes | 281 | 66.6 |
| No | 128 | 30.3 |
| Not specified | 13 | 3.1 |
Association between the desire to procreate and socio-demographic and clinical factors. N: number. PR: prevalence ratio. 95% CI: 95% confidence interval.
| Fertility Desire (N=329) | No Fertility Desire (N=93) | PR | 95% CI | P | |
|---|---|---|---|---|---|
| Age Brackets | |||||
| <40 years | 268 (81%) | 51 (55%) | 1.42 | [1.42-1.68] | <0.001 |
| >40 years | 61 (19%) | 42 (45%) | |||
| Sex | |||||
| Female | 268 (81%) | 69 (74%) | 1.11 | [0.96-1.28] | 0.12 |
| Male | 61 (19%) | 24 (26%) | |||
| School Educational Level | |||||
| Primary and secondary | 265 (80%) | 75 (81%) | 1.00 | [0.88-1.13] | 0.98 |
| University | 64 (20%) | 18 (19%) | |||
| Marital Status | |||||
| Single | 155 (47%) | 46 (58%) | 0.92 | [0.84-1.02] | 0.09 |
| Married or coupled | 174 (53%) | 34 (42%) | |||
| Parent of a Child Status | |||||
| Yes | 255 (77%) | 88 (95%) | 0.79 | [0.73-0.86] | <0.001 |
| No | 74 (23%) | 5 (5%) | |||
| Number of Children | 1.7 | 3.2 | <0.001 | ||
| Partner Desire | |||||
| Yes | 197 (60%) | 22 (24%) | 1.38 | [1.24-1.54] | <0.001 |
| No | 132 (40%) | 71 (76%) | |||
| Adoption | |||||
| Yes | 163 (49.5%) | 36 (39%) | 1.10 | [0.99-1.22] | 0.06 |
| No | 166 (50.5%) | 57 (61%) | |||
| Professional Activity | |||||
| Yes | 133 (40%) | 40 (43%) | 0.98 | [0.88-1.08] | 0.65 |
| No | 196 (60%) | 53 (57%) | |||
| Loss of Weight >10% | |||||
| Yes | 144 (44%) | 55 (59%) | 0.87 | [0.79-0.97] | <0.001 |
| No | 185 (56%) | 38 (41%) | |||
Clinical and Therapeutic Data of the Study Population
Prior to our survey, 43.6% (184/422) of patients were screened when they presented suspect clinical signs of AIDS (data not shown); one-third [32.0% (135/422)] of patients were associated with opportunistic infections. The proportion of patients included during voluntary screening was 26.8% (113/422), and 11.1% (47/422) patients were screened because of the HIV-positive status of a family member. Clinically, patients were diagnosed for depression, weight loss, and skin lesions in proportions of 71.6% (302/422), 47.2% (199/422), and 32.5% (137/422), respectively. ART was ongoing for 82.9% (350/422) of patients, with grade 3 and 4 side effects reported in 67.3% (284/422) of cases (data not shown).
Knowledge of HIV Infection and MAP
Inquiry into the knowledge of mothers about HIV showed that 89.8% (379/422) had received information about HIV and mother-to-child virus transmission. Fifty percent (211/422) were informed about ART and fetal toxicity, and 73.2% (309/422) were told about the necessity to refrain from breastfeeding. Only 16.1% (68/422) and 10.1% (45/422) of the patients received information concerning the MAP or/and MAP method, with very few [1.4% (6/422)] patients who solicited MAP within hospital, so as to be assisted in their desire to procreate (data not shown).
Desire to have Children Among Patients Living with HIV Infection
The desire to have children was expressed by 78% (329/422) of patients, and the possibility of further adoption was found in 47.2% (199/422) of patients (Table 1). The willingness to have an HIV-positive child and the motivation to assume this responsibility was observed in 66.6% (281/422) of individuals (Table 1). Among the 329 patients wishing to have children, HIV sero-discordant couples accounted for 33.4% (110/329) of patients, and 82.4% (271/329) were treated with antiretroviral drugs (data not shown). Among the 329 patients with the desire to have children, the following reasons prevailed: insufficient numbers of children born to the patient [18.8% (62/329)], the desire to be a parent [17.8% (75/329)], the role of child-bearing [15.2% (50/329)], assertiveness [12.5% (41/329)], or satisfaction of the spouse [11.2% (37/329)] (data not shown).
In cases of impaired health status during pregnancy, 22.8% of the 272 women interviewed preferred to keep their pregnancy. Among them, only 11.9% reported visiting a doctor, while 10.2% admitted to having an abortion or wanting to commit suicide (data not shown). The influence of the familial environment on PLHIV’s desire for a child was also analyzed (data not shown). Parents often encouraged the patient's desire for children in 26.1% cases, especially when they were informed about the patient's HIV status beforehand. Indeed, their sex partners shared the desire for children in 60.0% cases when they were informed about the patient’s HIV status (data not shown).
We analyzed the relationships between the desire to have a child by PLHIV and socio-demographic, clinical, therapeutic, and epidemiological factors (Table 2). The results showed that the desire for children was significantly higher in subjects under 40 years of age compared to those over 40 years of age [81%(268/329) versus 19%(61/329), p<0.001]. The average number of children was significantly lower for patients wishing to have children than for the other patients (1.7 versus 3.2, p<0.001).
However, the frequency of the desire for children was significantly higher when the desire was shared by the couple [77%(255/329) versus 23%(74/329), p<0.001], or in patients who had a partner with parental desire [60%(197/329) versus 40%(132/329), p<0.001].
Concerning the associations between child desire in PLHIV and clinical parameters, a significant result was observed only with weight loss: the desire to procreate was significantly higher in patients that were apparently in shape when compared to those of lower weight 56% (185/329) versus 44% (144/329), p<0.001 (Table 2). No significant relationship was observed between the desire for children and the other parameters including sex, marital status and educational level, practice of adoption, employment status, condom use, and ART therapy.
Concerning the associations between child desire in PLHIV and clinical parameters, a significant result was observed only with weight loss: the desire to procreate was significantly higher in patients that were apparently in shape when compared to those of lower weight [56%(185/329) versus 44%(144/329), p<0.001] (Table 2). No significant relationship was observed between the desire for children and the other parameters including sex, marital status and educational level, practice of adoption, employment status, condom use, and ART therapy.
DISCUSSION
We conducted this pilot study in Gabon, one of the first in sub-Saharan countries, to study the overall socio-demographic and behavioral factors associated with the desire for procreation among patients living with HIV. The study took place against a background of increasing numbers of HIV-infected patients screened between 1996 and 2011, across three study sites, while the HIV prevalence was stabilized in Gabon [13-15]. This stabilization can be explained by the health ministry’s policy and the medical team’s efforts to increase the HIV infection screening in asymptomatic individuals. These actions are in concordance with the World Health Organization’s recommendations, which hold the objective of developing preventive methods and strategies for antiretroviral treatment accessibility while benefiting the largest possible number of HIV-infected patients.
In contrast to previous studies that featured male predominance, ours results showing female predominance in HIV-infected patients were in concordance with previous studies conducted in Gabon and other sub-Saharan African countries [13, 14, 16-18]. This discrepancy can be explained by the fact that our recruitment was done on a voluntary basis, whereas it is known that in African culture in general, and particularly in Gabon, that women are more sensitive to questions related to procreation [6, 8].
Indeed, women’s infertility is often a source of social discrimination in African countries. As has been previously described, young women aged from 20-40 years old, those without professional activities, and those living below the poverty line were the most represented [6-8, 13, 14, 15, 17, 19, 20]. These data highlight the possible exposure of young adults most concerned by procreation needs to HIV transmission in the absence of preventive measures available to HIV-infected patients or sero-discordant couples. Otherwise, it appears that relatively uneducated patients were predominant in our study, rather than those with a university-level education. This observation reflects the fact that the general population’s education level in Gabon [13, 14, 21] is unlike that of similar African studies [17,18, 21]. It has been shown that irrespective of the form of the adopted union, communication between spouses increased with the partners' educational level, and reproductive health indicators were better if there was more dialogue between the couple’s partners [17, 18, 21]. This refers to the idea that one’s level of education as a key factor in the behavior of individuals when searching for information, seeking care, and adhering to treatment.
In our study, the addition of patients with a secondary school- or university-level education represented a large majority of the study population. This observation, as well as the treatment of HIV-infected patients with antiretroviral drugs, could explain the new needs and expectations observed in this young population, as they have a scholarly and educational disposition to become involved in the national development of projects that provide assistance methods for procreation and family planning programs.
The majority of patients were cohabiting or single. This might be explained by the patients’ youth or AIDS sero-positivity, which may cause the rupture or death of one partner and result in difficulty when beginning new relationships or re-establishing a new family. It has been shown that the HIV spread is higher in patient populations with multiple sexual partners and a lack of condom usage during sexual intercourse [13, 14, 21]. The proportion of patients using condoms was less when compared to Swiss HIV cohort observations [22], and sexual behavior following the announcement of their HIV status was variable.
Although our results show that the majority of sexual intercourse was protected, 13.3% of patients did not use condoms consistently during every sexual activity. HIV transmission is known to be associated with the lack of condom usage, and HIV-positive childbirths can be reduced by using contraceptive methods [23-26]. These were practiced by only one-third of patients with a sexual partner in our study. This observation might be explained by the fact that women may lack information about contraception, as has been shown in several studies; specifically, contraceptive methods are increasingly used when women are exposed to mass media information or family planning [19,20, 23, 24]. These results strongly suggest that the promotion of contraception should be a part of strategies to reduce mother-to-child HIV transmission. On the other hand, one-third of sero-discordant couples do not know the HIV status of their partner. The main reasons for this included a lack of discussion, the absence of marriage plans, and the fear of the partner’s reaction after the announcement of his or her HIV status in new relationships.
Therefore, the sero-discordance is problematic since it alters the couple’s balance by creating tension and affecting partner intimacy [20, 23-26]. Moreover, we noticed that more than half of patients lived as married or unmarried couples. These life conditions constitute an appropriate familial environment where interventions for MAP can be carried among PLHIV or sero-discordant couples.
Of note, in the current Gabonese study, the majority of patients (78%) had a desire for children as compared to patients from Uganda (7%), Lesotho (39%), Ethiopia (45.5%), or Nigeria (54.9%) [15, 17, 26-29]. To date, we have no clear scientific explanation regarding the differences in the frequency of patients with a desire for fertility between African countries. A multi-center study analyzing cultural, religious, socio-demographic, and economic factors, as well as that includes infrastructures and hospital organizations, would be useful for understanding these differences, since the population of patients with the desire to have a child exhibited the same characteristics in these different African studies (ie, a young female population with 1 to 2 children, with a low educational level, and without the influence of professional activities).
The reasons to have children, as given by the patients wishing to have children, included the role of every person to ensure his or her lineage, the pleasure of being a parent, the desire to have many children, and assertiveness despite illness.
In addition, the majority of patients were ready to have a child with HIV if this was to happen, but they would first take every precaution to minimize the risk of HIV transmission to the child. Among patients with an impaired health status during pregnancy, it is clear from our analysis that only 10% of patients admitted to wanting an abortion or to commit suicide. In contrast, the majority preferred to keep their pregnancies and to seek medical attention if there was a severe deterioration in their health. Otherwise, the opinion of the patients’ social environment also influenced their desire to procreate. Half of the patients with a partner wanted children, while one-third of them would encourage the patients’ desires to procreate, especially when they were informed of their HIV status. Thus, the PLHIV’s desire for children found a favorable echo from their entourage, especially from their sexual partners, which could also facilitate the promotion of the MAP.
Regarding correlations between the desire to procreate and socio-demographic parameters, no association was observed between sex, educational level, antiretroviral treatment, and the marital status of patients, while the proportion of married women who had the desire to have children was higher than among single women, as previously described [15, 21, 26]. Indeed, the desire to procreate was particularly high if partners also wished to have children (especially among patients aged under 40 years), and this was associated with a small number of children [23, 25-27].
However, many couples said that they wanted to be advised by a healthcare professional before conceiving a child. The desire for children remains disturbed by the fear of HIV transmission to the HIV-negative partner in discordant couples [18, 19, 24]; however, it is associated with marital life, partner consent, and the absence of weight loss. Accordingly, the desire to procreate was common among young HIV-infected patients taking or not taking ART. Interestingly, the knowledge of the risk of HIV transmission to children, as well as preventive measures, seems to be acquired by the majority of patients, while measures of MAP were generally unknown.
CONCLUSION
Our observations highlight the need to further integrate HIV/AIDS support into family planning programs to assist PLHIV and sero-discordant couples with their desire to have children. These initial data regarding the desire to procreate in HIV-infected patients living in Gabon could serve to justify the creation of MAP for PLHIV and sero-discordant couples among health professionals and health authorities, followed by the objective of reducing the risk of mother-to-child HIV transmission.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We thank Constantin Fesel for contribution to writing and English correction of the manuscript. English-language editing of this manuscript was provided by Journal Prep.


