All published articles of this journal are available on ScienceDirect.
HIV Co-infection Increases Mortality and Impairs Functional Independence and Physical Performance in Hospitalized Tuberculosis Patients
Abstract
Introduction
Tuberculosis (TB) and Human Immunodeficiency Virus (HIV) infection have been found to impact physical function significantly. However, data regarding the effect of TB/HIV co-infection on functional status remain limited. This study aimed to assess the impact of HIV co-infection on the functional independence and physical performance of TB patients during hospitalization, and associated mortality.
Methods
This cross-sectional study included hospitalized TB patients from the Brazilian infectious diseases reference center. Their sociodemographic and clinical characteristics were recorded. Functional independence was assessed using the Functional Independence Measure (FIM), and physical performance was evaluated with the Short Physical Performance Battery (SPPB).
Results
A total of 49 patients were included: 22 with TB/HIV co-infection and 27 with TB-only. The TB-only group showed significant increases in total FIM scores (p=0.027) and SPPB (p = 0.001) at discharge compared to admission, which was not observed in the TB/HIV co-infected group. Mortality occurred only in the TB/HIV co-infected group (p=0.01).
Discussion
This study demonstrated that HIV co-infection impaired functional independence and physical performance in TB patients during hospitalization. This impairment was associated with poorer clinical outcomes, including elevated mortality, which aligns with previously documented HIV-related functional deficits. Our findings, which reveal higher mortality among co-infected individuals, are consistent with the widely recognized role of functional limitations in predicting poorer patient outcomes.
Conclusion
The present study highlights the detrimental effect of HIV co-infection on both functional outcomes and survival in hospitalized TB patients. This underscores the urgent need for integrated care strategies to enhance functional outcomes and reduce mortality in this population.
1. INTRODUCTION
Tuberculosis (TB) remains a major global public health challenge, ranking as a leading cause of morbidity and the second most lethal infectious disease worldwide, surpassed only by COVID-19 and exceeding the mortality burden of Human Immunodeficiency Virus (HIV)/Acquired Immunodeficiency Syndrome (AIDS) [1]. According to the World Health Organization (WHO), an estimated 10.6 million people developed TB in 2021, resulting in 1.6 million deaths, including approximately 187,000 among patients living with HIV. HIV co-infection is the most substantial known risk factor for both the development of active TB and the reactivation of latent TB infection [2]. Individuals living with HIV are approximately 18 times more likely to develop active TB when compared to those without HIV [1]. Conversely, TB increases HIV viral replication at the site of Mycobacterium tuberculosis infection, thereby accelerating HIV disease progression as well as the onset of AIDS [3].
Although Mycobacterium tuberculosis primarily targets the lungs and causes diverse patterns of pulmonary damage, it can also affect different human systems, leading to systemic symptoms, such as fever, fatigue, loss of appetite, and weight loss. Additionally, peripheral muscle strength is also often compromised in TB patients. Muscle weakness is a key feature of cachexia, a hallmark of pulmonary TB, which is characterized by severe, disproportionate muscle wasting, leading to progressive weight loss, fatigue, and reduced muscle function [4]. Consequently, impaired muscular function leads to lower exercise tolerance, reduced daily physical activity, and impaired quality of life [5]. Physical function limitations are also observed in patients with HIV without TB co-infection, even in those with effectively treated infection [6, 7]. Although the literature provides extensive information on the physical functioning of patients with either TB or HIV infection, the impact of TB/HIV co-infection on functional status remains poorly understood. Therefore, this study aimed to assess the impact of HIV co-infection on functional independence and physical performance among hospitalized TB patients, as well as to investigate the associated mortality rate.
2. MATERIALS AND METHODS
2.1. Design and Ethics Approval
This cross-sectional study was conducted between January 2021 and September 2021 at the Hospital de Doenças Tropicais Dr. Anuar Auad, a reference center for infectious diseases in the center-west region of Brazil. The study protocol received approval from the Ethics Committee of the Hospital de Doenças Tropicais Dr. Anuar Auad (protocol number: 3.941.045), and written informed consent was obtained from all participants prior to enrollment.
2.2. Study Population
A non-probability convenience sample was employed due to the homogeneous characteristics of the population and the limited collection period. Patients were included in this study if they were hospitalized, at least 18 years old, had a suspected or confirmed TB diagnosis at the time of recruitment, were able to understand and respond to the study instruments, and were enrolled in standard hospital physiotherapy care. Patients were excluded if they had unavailable baseline data, refused to participate, or lacked a confirmed TB diagnosis.
2.3. Experimental Procedure
Sociodemographic characteristics, clinical condition data, and variables related to HIV infection were recorded at baseline. Moreover, functional independence was assessed by quantifying the patient's ability to perform activities of daily living (ADLs) using the Functional Independence Measure (FIM), which consists of two subscales: motor and cognitive. The motor subscale score ranges from 13 to 91, while the cognitive subscale score ranges from 5 to 35; the total score ranges from 18 to 126 [8]. Physical performance was assessed using the Short Physical Performance Battery (SPPB), which combines results from three tests: usual paced 4-meter walking velocity, time to rise from a seated position five times, and static standing balance [9]. Each test is scored from 0 to 4, with a total score ranging from 0 (worst performance) to 12 (best performance). FIM and SPPB data were recorded for each patient at hospital admission (within 72 hours) and discharge.
2.4. Sample Size
A priori power analysis was conducted using G*Power to determine the minimum required sample size for detecting within-group changes in SPPB scores using the Wilcoxon signed-rank test for matched pairs. The calculation assumed a Laplace distribution, which better accounts for outliers and heavier tails often observed in clinical data. The analysis was based on a moderate effect size (dz = 0.5), an alpha error probability of 0.05, a one-tailed test, and a desired power of 0.80. The result indicated that a minimum total sample size of 18 participants would be required to detect significant differences with sufficient statistical power. The actual achieved power under these conditions was 81.18%.
2.5. Data Analysis
Descriptive statistics were used to characterize the patient population and assess differences between the TB-only group and the TB/HIV co-infected group. Categorical variables were analyzed descriptively and presented as absolute (n) and relative (%) frequencies. Numerical variables are represented as mean and standard deviation. The comparison of proportions was performed using Fisher's exact test or the chi-squared test. The Mann-Whitney test was carried out to compare differences between the TB-only and TB/HIV co-infected groups (intergroup analysis). The Wilcoxon test was conducted to assess changes within each group between admission and discharge (intragroup analysis). The level of significance was set at p <0.05. A commercial statistical software was used for all statistical analyses (Stata, version 14).
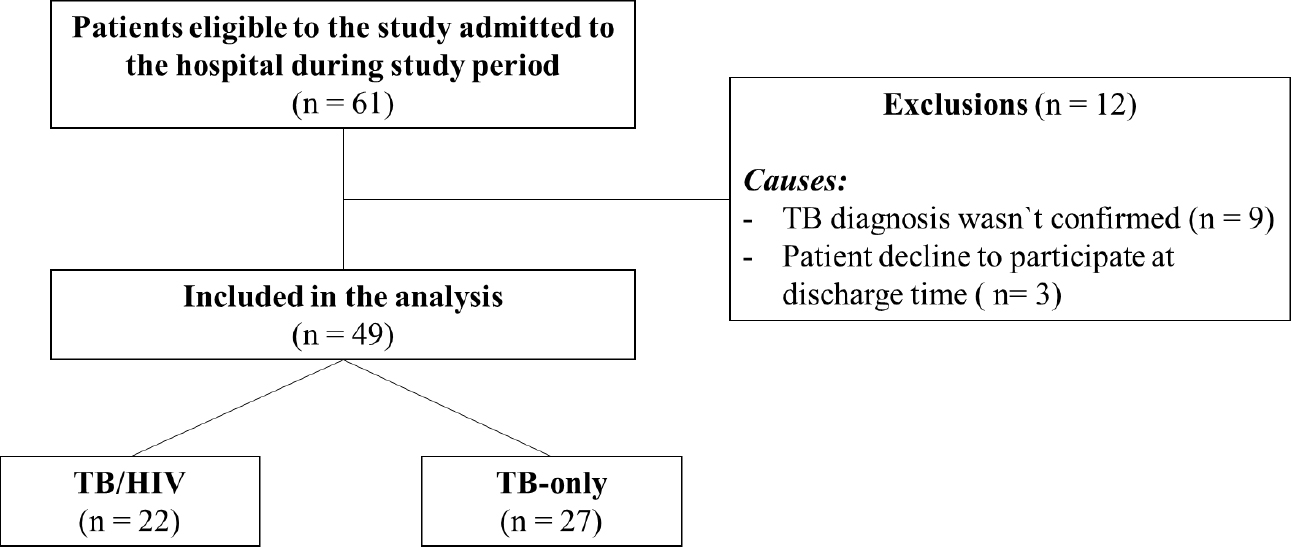
A flowchart showing the overview of the patients enrolled in the data analysis.
3. RESULTS
3.1. Socio-demographic and Clinical Characteristics
Out of 61 eligible patients hospitalized with a confirmed or suspected TB diagnosis between January 2021 and September 2021, nine patients were excluded due to unconfirmed TB diagnoses, and three declined participation. Consequently, 49 patients were included in the analysis, comprising 22 with TB/HIV co-infection and 27 with TB-only (Fig. 1). Baseline characteristics were similar between groups; however, all deaths occurred in the TB/HIV co-infected group, with four patients (18%) dying during hospitalization (p = 0.011) (Table 1).
3.2. HIV Infection
Among the 22 TB patients co-infected with HIV, 11 (50%) were diagnosed with HIV at least 12 months prior to data collection. The remaining 11 patients were diagnosed with HIV for up to 12 months prior to data collection. At the time of hospitalization, most TB/HIV co-infected patients exhibited elevated viral loads (>100,000 copies) (n = 10; 52.63%), and a low CD4 count (<200 cells/mm3) was also prevalent (n = 16; 80%). A total of seven TB/HIV co-infected patients were taking antiretroviral therapy (ART) irregularly, and six had completely discontinued treatment (Table 1).
| Variables |
TB-only Infected (n = 27; 55.1%) |
TB/HIV co-Infected (n = 22; 44.9%) |
p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age (years) | |||||
| 18-30 | 8 | 29.63 | 4 | 18.18 | 0.098 |
| 31-59 | 13 | 48.15 | 17 | 77.27 | |
| ≥60 | 6 | 22.22 | 1 | 4.55 | |
| Sex | |||||
| Male | 22 | 81.48 | 18 | 81.82 | 1.000 |
| Female | 5 | 18.52 | 4 | 18.18 | |
| Education level (years) | |||||
| 0-4 | 7 | 25.92 | 6 | 27.27 | 0.441 |
| 5-8 | 10 | 37.03 | 3 | 13.64 | |
| 9-11 | 7 | 25.92 | 8 | 36.36 | |
| >11 | 1 | 3.70 | 0 | 0 | |
| Non-informed | 2 | 7.41 | 5 | 22.73 | |
| Social Group | |||||
| Employed | 14 | 51.85 | 13 | 59.09 | 0.879 |
| Unemployed | 3 | 11.11 | 4 | 18.18 | |
| Retired | 5 | 18.52 | 3 | 13.64 | |
| Homeless | 4 | 14.81 | 2 | 9.09 | |
| Deprived of freedom | 1 | 3.70 | 2 | 9.09 | |
| Per capita income (minimum wage) | |||||
| < 1 | 23 | 85.19 | 17 | 77.27 | 0.565 |
| 1 - 2 | 4 | 14.81 | 4 | 18.18 | |
| 3 - 4 | 0 | 0 | 1 | 4.55 | |
| Length of hospital stay (days) | |||||
| 1 -7 | 9 | 33.33 | 5 | 22.73 | 0.572 |
| 8 -15 | 9 | 33.33 | 10 | 45.45 | |
| 16 – 30 | 3 | 11.11 | 5 | 22.73 | |
| 30 – 45 | 3 | 11.11 | 1 | 4.55 | |
| > 45 | 3 | 11.11 | 1 | 4.55 | |
| Clinical form of TB | |||||
| Pulmonary TB | 21 | 77.78 | 17 | 77.27 | 1.000 |
| Extrapulmonary TB | 3 | 11.11 | 2 | 9.09 | |
| Mixed Type TB | 3 | 11.11 | 3 | 13.64 | |
| Acid-Fast Bacillus testing | |||||
| Positive | 13 | 48.15 | 9 | 40.91 | 0.862 |
| Negative | 7 | 25.93 | 7 | 31.82 | |
| Non-informed | 7 | 25.93 | 6 | 27.27 | |
| Hospitalization outcome | |||||
| Hospital discharge | 25 | 96.15 | 14 | 63.64 | 0.011 |
| Hospital transference | 1 | 3.85 | 4 | 18.18 | |
| Death | 0 | 0 | 4 | 18.18 | |
| HIV Diagnosis time (month) | |||||
| > 1 | - | - | 1 | 4.55 | N/A |
| 1 - 6 | - | - | 7 | 31.82 | |
| 6 - 12 | - | - | 3 | 13.64 | |
| ≥ 12 | - | - | 11 | 50.00 | |
| Viral load | |||||
| < 50 (undetectable) | - | - | 2 | 10.53 | N/A |
| < 10.000 | - | - | 4 | 21.05 | |
| 10.000 - 100.000 | - | - | 1 | 5.26 | |
| > 100.000 | - | - | 10 | 52.63 | |
| Non informed | - | - | 2 | 10.53 | |
| T CD4+ (cells/mm3) | |||||
| > 350 | - | - | 1 | 5.00 | N/A |
| 200-350 | - | - | 1 | 5.00 | |
| < 200 | - | - | 16 | 80.00 | |
| Non informed | - | - | 2 | 10.00 | |
| Adhesion to treatment | |||||
| Regularly | - | - | 9 | 40.91 | N/A |
| Irregularly | - | - | 7 | 31.82 | |
| Abandonment | - | - | 6 | 27.27 | |
| Parameters | TB-only Infected | p1-value | TB/HIV Co-infected | p2-value | p3-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Admission | Discharge | ∆ | Admission | Discharge | ∆ | ||||
| Mean (sd) | Mean (sd) | Mean (sd) | Mean (sd) | Mean (sd) | Mean (sd) | ||||
| FIM Domains | |||||||||
| Self-care | 36.08 (12.96) | 36.15 (12.99) | 0.08 (0.39) | 0.317 | 39.82 (7.37) | 38.24 (10.72) | -1.59 (7.08) | 0.966 | 0.653 |
| Sphincter control | 12.23 (4.01) | 12.23 (4.01) | 0.00 (0.00) | 0.999 | 12.65 (3.66) | 13.71 (0.69) | 1.06 (3.01) | 0.157 | 0.077 |
| Mobility | 17.65 (6.27) | 17.73 (6.29) | 0.08 (0.74) | 0.564 | 18.53 (4.77) | 18.24 (5.29) | -0.29 (1.49) | 0.966 | 0.688 |
| Locomotion | 11.19 (4.79) | 11.38 (4.78) | 0.19 (0.57) | 0.083 | 11.59 (4.29) | 11.71 (4.06) | 0.12 (0.33) | 0.157 | 0.947 |
| Motor | 77.15 (27.44) | 77.46 (27.46) | 0.31 (1.29) | 0.377 | 82.59 (18.75) | 80.06 (25.50) | -2.53 (7.41) | 0.516 | 0.287 |
| Comunication | 13.5 (1.17) | 13.62 (0.98) | 0.12 (0.82) | 0.978 | 13.53 (1.33) | 14.41 (1.70) | 0.88 (2.78) | 0.157 | 0.209 |
| Social cognition | 20.08 (1.90) | 20.15 (1.89) | 0.08 (0.39) | 0.317 | 19.82 (3.34) | 20.35 (2.67) | 0.53 (2.18) | 0.317 | 0.734 |
| Cognitive | 33.58 (2.69) | 33.77 (2.63) | 0.19 (1.20) | 0.978 | 32.76 (6.66) | 33.53 (6.06) | 0.76 (3.15) | 0.317 | 0.465 |
| Total | 110.73 (29.38) | 111.46 (29.69) | 0.73 (1.48) | 0.027 | 115.35 (25.29) | 114.35 (28.97) | -1.29 (3.85) | 0.898 | 0.046 |
| SPPB Domains | |||||||||
| Balance | 2.19 (1.33) | 2.46 (1.48) | 0.27 (0.45) | 0.008 | 2.21 (1.37) | 2.57 (1.40) | 0.36 (0.63) | 0.046 | 0.812 |
| Gait speed | 2.46 (1.82) | 3.00 (1.57) | 0.54 (1.21) | 0.014 | 2.86 (1.41) | 3.00 (1.41) | 0.14 (0.36) | 0.157 | 0.440 |
| Sit-to-stand | 2.92 (1.57) | 3.12 (1.56) | 0.19 (0.40) | 0.025 | 2.86 (1.51) | 3.29 (1.44) | 0.43 (0.94) | 0.084 | 0.714 |
| Total | 9.04 (3.26) | 10.18 (3.08) | 1.50 (2.46) | 0.001 | 9.25 (2.38) | 10.33 (1.72) | 1.08 (1.44) | 0.016 | 0.730 |
3.3. Functional Independence and Physical Performance
The TB-only group showed a significant increase in total FIM score at hospital discharge compared to admission (p = 0.027), which was not observed in the TB/HIV co-infected group. The gain in the total FIM score (discharge–admission) was also significantly higher in the TB-only group (0.73 points) compared to the TB/HIV co-infected group (-1.29 points) (p = 0.046). Similarly, the TB-only group exhibited significant improvements in each domain of the SPPB, i.e., balance test (p = 0.008), gait speed test (p = 0.014), sit-to-stand test (p = 0.025), as well as in the total SPPB score (p = 0.001) at discharge, compared to admission. On the other hand, the TB/HIV co-infected group showed a significant increase only in the balance test component of the SPPB test (p = 0.046) and in the total SPPB score (p = 0.016) (Table 2).
4. DISCUSSION
To our knowledge, this is the first study to compare functional independence and physical function between hospitalized patients co-infected with TB and HIV and those infected with TB only. We demonstrated that HIV co-infection significantly increased mortality and negatively impacted both functional independence and physical function in patients with TB during hospitalization. The demographic characteristics of this cohort were predominantly male, characterized by low levels of education, and a high prevalence of vulnerable living conditions, such as unemployment, homelessness, or incarceration. Among those employed, the majority reported low income levels. The demographic profile of our sample aligns with the Brazilian TB scenario [10], including average income and poverty levels, which are factors recognized by the WHO as key determinants of TB, particularly in the context of the coronavirus disease 2019 (COVID-19) pandemic [1].
In this study, we first evaluated functional independence using the FIM, a self-report instrument designed to evaluate an individual's ability to perform activities of daily living [8]. It was observed that in the TB-only infected group, the FIM score at hospital discharge significantly improved compared to the score at admission, which was not observed in the TB/HIV co-infected group. Following the FIM assessment, we conducted the SPPB, a specific and objective test widely used to evaluate physical performance, which also serves as a predictor of disability and mortality [11, 12].
In accordance with the FIM results, the TB-only infected group showed a significant increase in the scores obtained in each domain of the SPPB, such as balance, gait speed, and sit-to-stand, as well as in the total SPPB score at discharge compared to admission. This functional improvement during hospitalization in patients with TB-only can be attributed to comprehensive local hospital care, which integrates a multidisciplinary team approach, notably including consistent daily physiotherapy interventions. In contrast, the TB/HIV co-infected group did not show improvements in gait speed and sit-to-stand performance; it only exhibited an increase in the balance test domain of the SPPB, which corresponded with a lack of improvement in the FIM score. Collectively, these findings indicate that the presence of HIV infection alongside TB impedes enhancements in both functional independence and physical performance during hospitalization. Although no studies have directly compared physical function between patients with TB-only and those co-infected with TB/HIV, substantial evidence indicates that HIV infection contributes to functional impairment [7, 13].
It is known that HIV infection introduces early physical complications, including low muscle mass, reduced bone mineral density, and an increased risk of fractures [14], which can subsequently lead to functional impairment [6]. Although functional impairments in HIV/AIDS were initially attributed to AIDS or AIDS wasting syndrome [14], the use of ART has also been implicated in impairing physical performance through mitochondrial dysfunction and decreased muscle strength, leading to progressive skeletal muscle dysfunction [15]. Moreover, mitochondrial and muscle function may be further compromised by biochemical changes associated with HIV infection, such as carnitine deficiency [16]. Additional factors contributing to impaired performance in patients with HIV include the association between anemia and fatigue [17], as well as inspiratory muscle weakness, which may reduce exercise capacity [18]. In our study, both HIV-related and ART-related factors may have contributed to the reduced functional performance observed in TB/HIV co-infected patients, given that our sample comprised patients with high viral loads, low CD4 levels, and active ART use.
Consistent with the worst functional status observed in TB/HIV co-infected patients, mortality during hospitalization was exclusively recorded in this group. This finding aligns with the established role of functional limitations as strong predictors of disability and mortality [19]. Furthermore, it is known that HIV co-infection is associated with worsening TB treatment outcomes [1] and a significant increase in mortality risk by accelerating TB progression and impairing CD4 recovery. This immunological decline can lead to rapid HIV replication, facilitating progression to AIDS and death among affected individuals [20]. The high mortality rate among TB/HIV co-infected patients reported in our study, alongside similar findings in the literature, underscores the critical importance of WHO's guidelines advocating preventive TB treatment in patients living with HIV [1]. On the other hand, a recent study [21] demonstrated HIV status as a protective factor associated with successful TB treatment. Although this finding contrasts with numerous reports documenting poorer outcomes in TB-HIV co-infected patients, it was also found that HIV positive individuals often receive heightened medical attention and benefit from enhanced coordination among specialized healthcare units. This increased level of care and multidisciplinary collaboration may contribute to improved treatment success in this population [21].
This study provides novel and significant findings, demonstrating that HIV co-infection is associated with increased mortality, impaired functional independence, and diminished physical performance in TB patients during hospitalization. However, the study has several limitations. Patients were recruited from a single hospital, which may limit the generalizability of the results to other settings. Furthermore, the data were obtained from a limited sample size. It is also noteworthy that the study period coincided with the onset of the COVID-19 pandemic, leading to a decline in the number of people diagnosed and hospitalized with TB [1]. Moreover, the proportion of TB cases among people living with HIV has been steadily declining over recent years, making it challenging to recruit a larger number of TB/HIV co-infected individuals. Despite these limitations, this study showed significant differences in mortality rates, functional independence, and physical performance between hospitalized patients co-infected with TB/HIV and those infected with TB-only. To validate and extend these findings, future studies should involve multicenter trials with larger sample sizes across diverse clinical settings.
CONCLUSION
The present study highlights the significant adverse impact of HIV co-infection on the functional recovery of hospitalized TB patients. While patients with TB alone demonstrated notable improvements in functional independence and physical performance during the hospitalization, these improvements were not observed in the TB/HIV co-infected group. Additionally, the co-infected group exhibited a significantly higher mortality rate. These findings emphasize the detrimental effect of HIV co-infection on both functional outcomes and survival in TB patients, underscoring the urgent need for integrated care strategies targeting both infections in order to enhance functional outcomes and reduce mortality in this population.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: J.M.S. and O.C.O.L.: Study concept, design, analysis and interpretation; W.M.S.: Analysis and interpretation of results; D.N.C.L.: Data collection. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ADLs | = Activities of Daily Living |
| AIDS | = Acquired Immunodeficiency Syndrome |
| ART | = Antiretroviral Therapy |
| COVID-19 | = Coronavirus Disease 2019 |
| FIM | = Functional Independence Measure |
| HIV | = Human Immunodeficiency Virus |
| SPPB | = Short Physical Performance Battery |
| TB | = Tuberculosis |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Ethics Committee of the Hospital de Doenças Tropicais Dr. Anuar Auad (HDT) (#3.941.045).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this article is available from the Zenodo Repository, reference number 15859082, at the following link: https://zenodo.org/records/15859082.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Programas de Residência Multiprofissional e em Área Profissional da Saúde of the Secretaria de Estado da Saúde de Goiás (COREMU/SES/GO) for their valuable support. They would also like to extend their sincere thanks to the Hospital de Doenças Tropicais Dr. Anuar Auad for their assistance.


